Public Meeting of the Board of Directors – Thursday 25 September 2025
Public Meeting of the Board of Directors will be held at 9.30am on Thursday 25 September 2025 in the Inspire@ room at Horizon Leeds, 3rd Floor, 2 Brewery Wharf, Kendall Street, Leeds, LS10 1JR.
Agenda
Opening proceedings
| Item | Item title | Lead | Time |
| 1 | Apologies for absence (verbal) | Merran McRae | 9.30am |
| 2 | Sharing stories (verbal) | Community and Wellbeing Services | 9.35am |
| 3 | Declarations of interests and any declarations of conflicts of interest in any agenda item (enclosure) | Merran McRae | No time specified |
| 4 | Minutes of the meeting held on 31 July 2025 (enclosure) | Merran McRae | No time specified |
| 5 | Matters arising (verbal) | Merran McRae | No time specified |
| 6 | Actions outstanding from the public meetings of the Board of Directors (enclosure) | Merran McRae | 10.05am |
Use of resources
| Item | Item title | Lead | Time |
| 7 | Chief Executive’s report (enclosure) | Dr Sara Munro | 10.10am |
| 8 | Report from the Chair of the Finance and Performance Committee for the meetings held on 23 September 2025 (to follow) | Cleveland Henry | 10.20am |
| 9 | Report from the Chief Financial Officer (enclosure) | Dawn Hanwell | 10.30am |
| 10 | Report of the Chief Operating Officer (enclosure) | Joanna Forster Adams | 10.40am |
| 10.1 | Winter Plan Board Assurance Statement (enclosure) | Joanna Forster Adams | 10.50am |
| Not applicable | Break | Not applicable | 10.55am |
Patient centred care
| Item | Item title | Lead | Time |
| 11 | Report from the Chair of the Quality Committee for the meeting held on 11 September 2025 (enclosure) | Dr Frances Healey | 11.10am |
| 12 | Report from the Director of Nursing and Professions (enclosure) | Nichola Sanderson | 11.15am |
| 12.1 | Safer Staffing Report (enclosure) | Nichola Sanderson | 11.25am |
| 12.2 | Establishment Review (enclosure) | Nichola Sanderson | 11.30am |
| 13 | Guardian of Safe-working Hours Q1 and Annual Report (enclosure) | Dr Chris Hosker | 11.40am |
Workforce
| Item | Item title | Lead | Time |
| 14 | Report from the Chair of the Workforce Committee for the meeting held on 7 August 2025 (enclosure) | Zoe Burns-Shore | 11.45am |
| 15 | Equality Annual Report (including WRES and WDES and Gender Pay Gap) (enclosure) | Darren Skinner | 11.50am |
Governance
| Item | Item title | Lead | Time |
| 16 | Report from the Chair of the Mental Health Legislation Committee for the meeting held on 5 September 2025 (enclosure) | Kaneez Khan | 12.10pm |
| 17 | Board of Directors Terms of Reference (enclosure) | Merran McRae | 12.15pm |
| 18 | Use of Trust Seal (verbal) | Merran McRae | No time specified |
| 19 | Any other business | Merran McRae | 12.20pm |
The next meeting of the Board will be held on Thursday 27 November 2025 at 9.30am in the Inspire@2 room at Horizon Leeds, 3rd Floor, 2 Brewery Wharf, Kendall Street, Leeds, LS10 1JR.
Declaration of Interests for members of the Board of Directors
Executive Directors
| Name | Directorships, including Non-executive Directorships, held in private companies or PLCs (with the exception of those of dormant companies). | Ownership, or part-ownership, of private companies, businesses or consultancies likely or possibly seeking to do business with the NHS. | Majority or controlling shareholdings in organisations likely or possibly seeking to do business with the NHS. | A position of authority in a charity or voluntary organisation in the field of health and social care. | Any connection with a voluntary or other organisation contracting for NHS services. | Any substantial or influential connection with an organisation, entity or company considering entering into or having entered into a financial arrangement with the Trust, including but not limited to lenders or banks. | Any other commercial or other interests you wish to declare. This should include political or ministerial appointments (where this is information is already in the public domain – this does not include personal or private information such as membership of political parties or voting preferences) | Declarations made in respect of spouse or co-habiting partner |
| Sara Munro Chief Executive |
Interim Chief Executive Officer Leeds Community Healthcare NHS Trust | None. | None. | Trustee Workforce Development Trust |
None. | None. | None. | None. |
| Dawn Hanwell Chief Financial Officer and Deputy Chief Executive |
None. | None. | None. | None. | None. | None. | None. | None. |
| Chris Hosker Medical Director |
Director Trusted Opinion Ltd. |
None. | Director Lilac Tree Clinic Ltd. |
None. | Director Lilac Tree Clinic Ltd. |
None. | None. | Partner: Director Trusted Opinion Ltd. |
| Joanna Forster Adams Chief Operating Officer |
None. | None. | None. | None. | None. | None. | None. | Partner: Director of Public Health Middlesbrough Council and Redcar and Cleveland Borough CouncilPartner: Chair The Junction Charity |
| Nichola Sanderson Director of Nursing and Professions |
None. | None. | None. | None. | None. | None. | None. | None. |
| Darren Skinner Director of People and Organisational Development |
Director Skinner Consulting Ltd. |
None. | None. | None. | None. | None. | None. | None. |
Non-Executive Directors
| Name | Directorships, including Non-executive Directorships, held in private companies or PLCs (with the exception of those of dormant companies). | Ownership, or part-ownership, of private companies, businesses or consultancies likely or possibly seeking to do business with the NHS. | Majority or controlling shareholdings in organisations likely or possibly seeking to do business with the NHS. | A position of authority in a charity or voluntary organisation in the field of health and social care. | Any connection with a voluntary or other organisation contracting for NHS services. | Any substantial or influential connection with an organisation, entity or company considering entering into or having entered into a financial arrangement with the Trust, including but not limited to lenders or banks. | Any other commercial or other interests you wish to declare. This should include political or ministerial appointments (where this is information is already in the public domain – this does not include personal or private information such as membership of political parties or voting preferences) | Declarations made in respect of spouse or co-habiting partner |
| Merran McRae Chair |
Director Finnbo Ltd |
None. | None. | None. | None. | None. | None. | Partner: Director Finnbo Ltd |
| Zoe Burns-Shore Non-executive Director |
Executive Director for Customer Delivery Money and Pensions Service |
None. | None. | None. | None. | None. | None. | None. |
| Frances Healey Non-executive Director |
None. | None. | None. | Trustee The National Confidential Enquiry into Patient Outcome and Death (NCEPOD) |
None. | None. | Visiting Professor University of LeedsAdvisory Role and Peer Reviewer Research studies and potential research studies related to patient safety |
None. |
| Cleveland Henry Non-executive Director |
Director 63 Argyle Road Ltd. |
None. | None. | Chair of the Board of Trustees Community Foundations for Leeds |
None. | None. | Director of Group Delivery & Deployment Optum (UK) (Digital Health sector) |
Partner: Lead Cancer Nurse Leeds Teaching Hospitals NHS Trust |
| Kaneez Khan Non-executive Director |
Director Primrose Consultancy Yorkshire |
None. | None. | None. | None. | None. | None. | None. |
| Katy Wilburn Non-executive Director |
None. | None. | None. | None. | None. | None. | None. | None. |
| Martin Wright Non-executive Director |
None. | None. | None. | Trustee Roger’s Almshouses (Harrogate) |
None. | None. | None. | Partner: Trustee Roger’s Almshouses (Harrogate) |
Declarations pertaining to directors being a Fit and Proper Person under the CQC Regulation 5 and meeting all the criteria in the Provider Licence and the Trust’s Constitution to be and continue to be a director
Each director has been checked in accordance with the criteria for fit and proper persons and have completed the necessary self-declaration forms to show that they do not fit within any definition of an “unfit person” as set out in the provider licence, the Health and Social Care Act 2008 (Regulated Activities) Regulations 2008 or the Trust’s constitution; that they meet all the criteria for being a fit and proper person as defined in the Social Care Act 2008 (Regulated Activities) Regulations 2008; and that there are no other grounds under which I would be ineligible to continue in post.
Executive Directors
| Criteria | Dr Sara Munro | Nichola Sanderson | Dawn Hanwell | Dr Christian Hosker | Joanna Forster Adams | Darren Skinner |
| a) Are they a person who has been adjudged bankrupt or whose estate has been sequestrated and (in either case) have not been discharged? | No | No | No | No | No | No |
| b) Are they a person who has made a composition or arrangement with, or granted a trust deed for, any creditors and not been discharged in respect of it? | No | No | No | No | No | No |
| c) Are they a person who within the preceding five years has been convicted of any offence if a sentence of imprisonment (whether suspended or not) for a period of not less than three months (without the option of a fine) being imposed on you? | No | No | No | No | No | No |
| d) Are they subject to an unexpired disqualification order made under the Company Directors’ Disqualification Act 1986? | No | No | No | No | No | No |
| e) Do they meet all the criteria for being a fit and proper person as defined in the Social Care Act 2008 (Regulated Activities) Regulations 2008. | Yes | Yes | Yes | Yes | Yes | Yes |
Non-executive Directors
| Criteria | Merran McRae | Zoe Burns-Shore | Kaneez Khan MBE | Dr Frances Healey | Cleveland Henry | Martin Wright | Katy Wilburn |
| a) Are they a person who has been adjudged bankrupt or whose estate has been sequestrated and (in either case) have not been discharged? | No | No | No | No | No | No | No |
| b) Are they a person who has made a composition or arrangement with, or granted a trust deed for, any creditors and not been discharged in respect of it? | No | No | No | No | No | No | No |
| c) Are they a person who within the preceding five years has been convicted of any offence if a sentence of imprisonment (whether suspended or not) for a period of not less than three months (without the option of a fine) being imposed on you? | No | No | No | No | No | No | No |
| d) Are they subject to an unexpired disqualification order made under the Company Directors’ Disqualification Act 1986? | No | No | No | No | No | No | No |
| e) Do they meet all the criteria for being a fit and proper person as defined in the Social Care Act 2008 (Regulated Activities) Regulations 2008. | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
Minutes for the Public Board of Directors Thursday 31 July 2025 at 9:30am
Held in the in Inspire@ room at Horizon Leeds, 3rd Floor, 2 Brewery Wharf, Kendall Street, Leeds, LS10 1JR.
Attendance
Board members
| Name | Role | Apologies |
| Mrs M McRae | Chair of the Trust | Attended |
| Mrs Z Burns Shore | Non-Executive Director | Sent apologies |
| Mrs J Forster Adams | Chief Operating Officer | Attended |
| Mrs D Hanwell | Chief Financial Officer and Deputy Chief Executive | Attended |
| Mr C Henry | Non-Executive Director (Senior Independent Director) | Attended |
| Dr F Healey | Non-Executive Director | Attended |
| Dr C Hosker | Medical Director | Attended |
| Ms K Khan MBE | Non-Executive Director | Attended |
| Dr S Munro | Chief Executive | Attended |
| Mr D Skinner | Director of People and Organisational Development | Attended |
| Miss N Sanderson | Director of Nursing and Professions | Attended |
| Miss K Wilburn | Non-Executive Director | Attended |
| Mr M Wright | Non-Executive Director (Deputy Chair of the Trust) | Attended |
All members of the Board have full voting rights.
Also in attendance
-
- Mrs C Edwards – Associate Director of Corporate Governance / Trust Board Secretary
- Mr K Betts – Corporate Governance Officer
- Ms Rachel Pilling – Carer Coordinator, Patient & Carer Experience Team (for minute 25/078)
- Mr Ian Dowd – Service User relative (for minute 25/078)
- Ms Amy Young – Occupational Therapist (for minute 25/078)
- Ms Annie Johnston – Senior Occupational Therapist (for minute 25/078)
- Dr Wendy Neil – Consultant Psychiatrist / Responsible Officer (for minute 25/084)
- Four governor / member of the public attended the meeting.
Minutes
Mrs McRae opened the public meeting at 09:30 and welcomed everyone.
25/077 – Apologies for absence (agenda item 1)
Apologies were received from Mrs Zoe Burns Shore, Non-Executive Director. The meeting was quorate.
25/078 – Sharing stories – Older People’s Service (agenda item 2)
Mrs McRae welcomed Mr Ian Dowd, a relative of a Service User of the Older People’s Service at The Mount, Ms Amy Young, Occupational Therapist, and Ms Annie Johnston, Senior Occupational Therapist.
Mr Dowd provided an overview of his family’s experience and his personal story of his mother who was admitted to The Mount in 2024. She was treated for both her mental health and medical issues and initially she was reluctant to engage with the staff. He highlighted the importance of the time provided to his mother by staff who all demonstrated care and compassion, and she was also supported by consistency and familiarity with the care staff. He noted that the multi-disciplinary team (MDT) meetings supported a holistic view of her care which was important in his mother’s treatment. The work between the clinical and pharmacy teams to support her physical health had a positive impact on mental health and she was supported to start small visits out and home. He noted she was now living independently back at home, and this was due to the time taken by all team to develop trust and familiarity with his mother to support her recovery journey.
Ms Young was the allocated occupational therapist for Mr Dowd’s mother and discussed the importance of getting to know service users and building a relationship. She noted how the team worked together to understand who would be best placed to develop a relationship with each service user. They work with the person rather than the diagnosis and understand their challenges and goals to support them to engage with the service and can learn a lot from their knowledge and life experience. They created environments that enabled service users to feel safe and empowered with choice and inclusion in their care planning to give them a sense of control over their recovery journey. She discussed the models of care used to support recovery with graded exposure to their home environment and self-care, highlighting the importance of the support provided at all stages of the recovery journey to ensure successful outcomes. She noted the importance of MDT meetings to bring together different perspectives and insight into each service users’ needs to make recovery more effective.
Ms Johnston highlighted the importance of sharing good practice within the service, including feedback from service users and carers, to ensure the teams provide a good service. The monthly OT development forums allowed good practice to be shared across teams, and they also network across teams to share good practice regarding all elements of the MDT.
Ms Young acknowledged the challenges to implementing good practice, with the main issue being time as there was a need to get to know the individual however the team was stretched, and it could be hard to give everyone the time they needed. She noted that resource demands could be a challenge and could impact on the team’s ability to deliver person centred care which impacted on consistency. Capacity and flow within the acute inpatient service was noted to impact on the ability for collaborative working, linking back to consistency for service users. There was also a risk of re-traumatisation, and the need to build trusting relationships to support recovery was key to managing this. She also noted that staff wellbeing and compassion was prioritised to support staff.
Mrs McRae thanked Mr Dowd for sharing his mother’s story, and thanked Ms Young and Ms Johnstone for showcasing the service provided and the personalised care focus. Mrs Forster Adams thanked them for attending and acknowledged the issues with time and patient flow which had been previously discussed at the Board, and the presentation had helped understand the service delivery element. She urged the team not to lose the authenticity of staff and teams to support development. She noted she would be keen to hear the feedback of the service for any Board support required.
Dr Healey commented the presentation had demonstrated the importance of involving the family in the MDT discussions, and the importance of understanding good practice with a need to hear more of these stories at a national level. Dr Munro acknowledged this and commented how hearing all the elements of the person-centred holistic care was important and inspirational and was a good tool to use for staff motivation and learning through sharing good practice and role modelling.
Ms Khan thanked the team for sharing the story and queried whether it was possible to provide that level of care and quality to all patients. Ms Young responded that every service user was at a different stage, so their needs were different therefore the entire case load was considered to deliver the care individuals required.
Mrs McRae reiterated her thanks to the team, and wished Mr Dowd and his family well, noting it was important to hear the positive story but also acknowledge the challenges faced.
The Board of Directors thanked everyone for attending the meeting and sharing the engagement work within the Older People’s Service.
25/079 – Declaration of interests for directors and any declared conflicts of interest in respect of the agenda items (agenda item 3)
Declaration of interests for directors and any declared conflicts of interest in respect of the agenda items (agenda item 3)
Dr Munro noted that there was a need to include her interim role as Chief Executive at Leeds Community Healthcare NHS Trust on the declarations of interest.
The Board of Directors noted that there would be an update to the declarations for Dr Munro. There were no other changes.
25/080 – Minutes of the previous meeting held on 29 May 2025 (agenda item 4)
The minutes of the meeting held on 29 May 2025 were received and agreed as an accurate record.
25/081 – Matters arising (agenda item 5)
The Board of Directors noted that there were no matters arising.
25/082 – Actions outstanding from the public meeting of the Board of Directors (agenda item 6)
Mrs McRae presented the action log which showed those actions previously agreed by the Board in relation to the public meetings, those that were completed and those that were still outstanding.
She noted that there were two actions ongoing within timeframe and that information had been circulated to address the action related to MSK data. Any queries were to be raised with Mr Skinner or via Workforce Committee.
The Board received the cumulative action log, agreed to close the actions that had been completed and noted the updates provided for ongoing actions.
25/083 – Action 29 supporting information – MSK Data (agenda item 6.1)
The Board received the additional information and noted the content.
25/084 – Annual RO and Medical Revalidation Report (agenda item 7)
Mrs McRae thanked Dr Neil, Responsible Officer, for attending. Dr Neil took the report as read by the Board and highlighted several points and priorities. She confirmed that 139 doctors had been recommended for revalidation which was a good position. She noted that work continued to develop the appraiser workforce, and the appraiser development forum provided inhouse bespoke support for the appraiser community across the Trust. She highlighted the work undertaken with the complaints team to move away from dealing with complaints related to medical staff generically to provide more individual responses to complainants and identify support for individual doctors. All medical line managers were approved case investigators which was positive, and the Trust was heavily involved in regional and national networks to share knowledge and good practice.
She noted that the priorities for the coming year focused on resources and the impact on the Trust’s ability to support an increased number of doctors within the Trust. This included those who were not directly connected to the Trust but worked within services as there was a need to include them in oversight processes. She noted that options to consider administrative support within the service had been challenging however there was a need to continue to offer high quality support and appraisals for doctors, and this was challenging with limited resource. She provided assurance to the Board on the delivery of requirements for medical revalidation however it was important to flag the resource issues. Mrs Hanwell noted that discussions would continue regarding the resource issue as there was a need to prioritise where resource was needed and consider urgent areas, acknowledging that the drive to employ more doctors brought a need for a review of resources.
Mrs McRae acknowledged the work that had gone into the process and thanked Dr Neil for the report. As Chair of the Board, she signed the report, and the Board noted the content of the report.
The Board received and noted the content of the Annual RO and Medical Revalidation Report.
25/085 – Report from the Chief Executive (agenda item 8)
Dr Munro presented the Chief Executive’s report, taking the content as read. She highlighted the engagement events that had taken place and had received an overwhelmingly positive response therefore would be followed by another round of events later in the year. She also noted the progress made by the procurement team which was positive and demonstrated that investing in the skills and capabilities of the team had improved the position.
She informed the Board about the visit from Dr Penny Dash, Chair of NHS England, in July 2025, where she met with ward teams and senior leadership teams which was well received.
In relation to the Leeds System Review, she updated the Board that phase 1 had been concluded including the initial stakeholder engagement work with partners, and it was now focusing on the next stage. The report would focus on recommendations including future provider partnerships in Leeds and links to the 10 Year Plan policy framework, with may include specific implications for organisations. She also acknowledged the retirement of Professor Phil Woods, Chief Executive of Leeds Teaching Hospitals NHS Trust.
She noted that, in relation to the 10 Year Plan, working groups had been established with membership including executive level colleagues. The aim was for the working group to develop draft documentation in September 2025, and she would keep the Board updated. She also noted that the future role of governors was unclear at the current time.
She highlighted the importance of the Reasons to be Proud including the work to support interns and apprenticeships within Estates and Facilities, linking to the 10 Year Plan and supporting people into employment.
Mr Wright noted that the 10 Year Plan was aspirational, and it would be important for the Board to have a development session in the future to review the detail and implications, although he acknowledged that there was more detail to be awaited. Dr Munro referred to the planned discussion for the private Board meeting, noting the headline statements regarding workforce changes, and expectations regarding Foundation Trusts and funding regimes including achieving a 3% surplus to fund investments, needed consideration. Mrs Hanwell added that the messaging could be contradictory within the plan therefore there was a need to review how it would be implemented and impact on the organisation. It was agreed that the planned autumn Board Development Session would include the 10 Year Plan to consider its implications.
Mr Henry noted the lack of delivery detail within the Plan, and that there was a need to consider how it is communicated and translated to set accurate expectations.
Mrs Hanwell noted that, in relation to phase two of the Leeds System Review, The Value Circle were linking with Directors of Finance to hold focused discussions regarding the estate elements raised.
Mrs McRae noted that there was organisational responsibility to influence the aspirations of the 10 Year Plan into delivery and that the Mental Health service framework was still being worked through. She thanked Dr Munro for the report.
The Board received the report from the Chief Executive and noted the content.
25/086 – Report from the Chair of the Finance and Performance Committee for the meetings held on 28 July 2025 (agenda item 9)
Mr Henry presented the Chair’s report from the Finance and Performance Committee meeting on 28 July 2025 and acknowledged that the reports from the Chief Operating Officer and Chief Financial Officer would cover some of the updates.
He highlighted the focus on the out of area placements and the financial position for the organisation. He noted the deterioration in physical health checks which was referred to the Quality Committee for further review. The Committee had discussed AI and suggested that there was a need for a further, deeper discussion by the Board to consider opportunities and challenges including any impact on the strategic risks. It had also reviewed the organisational priorities and been provided with assurance regarding the detail within the BAF.
He highlighted that the Data Security and Protection Toolkit had been reviewed, and that there was a need to bring forward a cyber EPRR session for the Trust. The Committee received the Care Service Delivery and Development Group Annual Report noting it was a large report, and discussion had taken place regarding the target audience.
In relation to disciplinary processes for BAME colleagues, this had been referred to the Workforce Committee for further review, and the clinically ready for discharge and flow work had been referred to the Mental Health Legislation Committee to discuss in more detail.
Mr Wright commented that in relation to AI the focus needed to be on ensuring that the appropriate governance was in place to provide assurance that it was being used appropriately. Mr Henry noted that data protection guidance did not change for AI therefore it should be considered alongside the existing framework. Mrs McRae acknowledged that encouraging curiosity was positive, but the use of it needed to be considered more be widely.
Miss Wilburn highlighted the national cost collection discussion that had taken place at the Committee, noting that the return had been completed for this year however it was acknowledged that it was flawed yet used in the Oversight Framework as a metric. It was therefore important to flag this risk to the Board. Mrs Hanwell responded acknowledging the risk however data quality in mental health across the metrics was an issue, and there was a need to improve the data collection across mental health including for the costing process.
Mrs McRae thanked Committee members and Mr Henry.
The Board of Directors received the Chair’s report from the Finance and Performance Committee and noted the matters reported on.
25/087 – Report from the Chief Financial Officer (agenda item 10)
Mrs Hanwell presented her Chief Financial Officer’s report, noting the discussion at Finance and Performance Committee. She highlighted that the Trust was on track with the plan acknowledging the improvement in the medical agency position. She noted that the run rate position was being delivered using nonrecurrent technical flex which was supporting the position for the Trust, therefore a recurrent set of balanced budgets were needed which was in progress. This would include a QIA process which would be undertaken in due course linked to the organisational priorities. She added that the estimate and assessment for the underlying position needed to be entered and medium-term planning commenced which would be shared in more detail as it was progressed through the Finance and Performance Committee.
He informed the Board that the system improvement target now included a mandatory requirement for each Place to take a share of the unidentified £33m. This had been undertaken through a stretch target for Leeds, agreed through the Strategic Finance Executive Group, for each provider to take £0.9m. The Trust would not be amending the current plan and would focus on non-recurrent savings starting in month 6. She noted she was confident that this could be achieved if all other plans were delivered.
She noted that the domains for the financial elements of the Oversight Framework were referenced within the report, and she was confident with the delivery of the finance domain at the current time, however there was no ability to move into a deficit position.
Mr Wright queried if the stretch element of the plan would be reported for Board purposes and Mrs Hanwell confirmed that this would be part of forecast reporting from month 6.
Mr Henry referred to the discussion at Finance and Performance Committee regarding oversight for negative impacts on service delivery because of the efficiencies required. Mrs McRae acknowledged that impacts would be seen but mitigation needed to be understood. Mrs McRae thanked Mrs Hanwell for the report.
The Board received the Chief Financial Officer’s report and noted the content.
2025 – 2026 Organisational Priorities Quarter 1 Progress Report (agenda item 11)
Mrs Hanwell presented the report noting the detail provided and that each Executive Director was responsible for a range of priorities. She highlighted the red alert regarding disciplinary numbers for BAME staff which had been referred to the Workforce Committee.
Mr Wright clarified the discussion at Finance and Performance Committee regarding the patient portal and assurance was provided that this would be back on track due to the work underway from a technical perspective.
Dr Munro noted that it was positive for the Workforce Committee to review the disciplinary data however noted that there had been an overall reduction in the number of disciplinaries with less staff in the process therefore the numbers were smaller. She commended the team for the reduction in numbers and providing appropriate support staff. Mr Henry noted that it had been referred as the percentage remained the same despite a reduction in numbers.
Mrs McRae thanked Mrs Hanwell for the report.
The Board of Directors received the 2025 – 2026 Organisational Priorities Quarter 1 Progress Report, and noted the content.
25/089 – Approval of the Data Security & Protection Toolkit (self-certification) (agenda item 12)
Mrs Hanwell presented the report noting the detail and discussion at Finance and Performance Committee. It was the first year this framework had been used which had resulted in added pressure on the outcome measures and level of detail required. The usual audit had been undertaken with one outcome not met, however an action plan had been put in place and the Trust was now approaching the standard required.
She highlighted the domain related to access and administration of system documentation which needed to be addressed. These were mainly finance and HR systems and whilst processes were robust the documentation required was not in place.
She noted that the national standards had not been met by several organisations therefore the focus would be on keeping the same standards next year to support organisations to deliver them before any changes were made.
Dr Healey commended the work and report but queried whether not updating the toolkit would lead to a potential risk that it would fall behind in terms of AI. Mr Henry commented that the standards remained the same whether AI was used or not which would ensure compliance.
Mrs McRae thanked Mrs Hanwell for the report.
The Board of Directors received the Data Security & Protection Toolkit (self-certification) and noted the content.
25/090 – Health and Safety Annual Report (agenda item 13)
Mrs Hanwell presented the report noting the detail provided and that it had been shared and discussed at the Audit Committee as part of the assurance and governance process. She noted that the integrated health and safety position had improved and whilst it was a complex area progress had been made with assurance provided on the work taken to date.
Dr Healey commended the progress made and referred to the detail within the Chair’s Report from the Audit Committee that discussions had taken place regarding the separating of patient and staff data, and work remained underway. She added that there was not yet a definition of what health and safety data included, and it needed to be based on a pragmatic review of Datix categories. She noted that the comments made at Audit Committee were to be included in the final version of the report. Mr Wright added that there were inconsistencies in the data provided to various Committees due to limitations of the system but this needed to be acknowledged within the final report. Mrs Hanwell confirmed that the appropriate amends would be made to the report as required and ongoing work regarding the Datix system was in place to support granularity of detail.
Mrs McRae thanked Mrs Hanwell for the report.
The Board of Directors received the Health and Safety Annual Report, and noted the content and assurance provided.
25/091 – Report of the Chief Operating Officer (agenda item 14)
Report of the Chief Operating Officer (agenda item 14)
Mrs Forster Adams presented her report, noting the depth of the discussion at Finance and Performance Committee. She noted that the report highlighted key areas of concern including patient flow and the out of area placement position, which had improved since the report was written but was still considerably off plan. She provided reassurance that the team were focusing on discharge and barriers to this, with discussions at Finance and Performance Committee noting that there was a need to systematise processes to support this, and appropriate accommodation to discharge people to remained an area of focus.
She highlighted that enteral feeding was noted within the report as it was a national issue. The leadership and commitment of the dietetic team had enabled individual service users to receive appropriate treatment, and alternatives were being provided where needed.
The recent resident doctor industrial action had finished the day before with an immediate offer to reengage in discussions, however there was a risk that action would continue over the coming months and move into other professional groups. She thanked all doctors who had provided cover on rosters during this time, supported by colleagues in the medical directorate. She noted that there were varying numbers involved in the action, alongside annual leave also being taken.
She drew attention to two new sections in the report detailing the significant improvements made within the Older People’s Service and Red Kite View following previous Board discussions.
Mrs Forster Adams noted the discussion regarding physical health checks at Finance and Performance Committee as following sustained improvements a deterioration had been seen, therefore work was underway to review this in detail. This would be shared via Finance and Performance Committee and Quality Committee when concluded.
Mr Wright noted the ongoing discussions with resident doctors and the impact of future strikes, and that the numbers of those taking strike action appeared to be higher compared to other industrial action. Mrs Forster Adams commented that there had been variation in the numbers in all previous action, with some numbers as high as over 70% taking part, therefore it could be variable. She added that variation this time had been between 37-49% which was consistent with previous episodes. She noted the continued discussions with the government and BMA however further episodes were expected.
Mrs McRae thanked Mrs Forster Adams for her report, noting the patient flow challenge however the report showed a continued commitment to improve the position. She noted if further support from the Board was required escalation processes could be used.
The Board received the Chief Operating Officer report and discussed the content.
EPRR (agenda item 15) and EPRR Assurance Standards (agenda item 15.1)
Mrs Forster Adams took the document as read and noted that the EPPR Annual Assurance Statement included a declaration regarding expertise and capacity to meet the duty and maintain compliance. The Trust achieved 74% compliance this year, which was non-compliant overall, however there was a plan in place to improve the position. She informed the Board that due to the small resource and team, including a vacancy since March 2025, she was not able to provide assurance regarding the capacity needed to meet the standard. She noted that work was underway to mitigate this with the support of colleagues outside the EPRR function, however she was unable to provide assurance that the standard would be maintained. It was under constant review by the Executive Team and if the position deteriorated support would be requested.
Mr Wright queried if consideration had been given to combining the function across Trusts to support the team capacity overall. Mrs Forster Adams responded that whilst this would provide resilience across partner organisations, the expertise and capacity may not change as there was a limited EPRR resource across other organisations. Dr Munro added that resilience remained low across all organisations against ever increasing national standards for EPRR.
Mrs McRae noted that as the lead Non-Executive Director for EPRR, she shared the capacity concerns raised and that she understood the caveat regarding assurance and acknowledged the reviews across the system regarding the potential to combine resources. She thanked Mrs Forster Adams for her report.
The Board received and approved the EPRR Assurance Standards.
25/093 – EPRR Annual Report (agenda item 15.2)
Mrs Forster Adams took the document as read and noted it had been reviewed at Finance and Performance Committee previously. It provided a summary of activity within the EPRR team across the last year and there were no areas of escalation.
Mrs McRae thanked Mrs Forster Adams for her report.
The Board received and accepted the EPRR Annual Report.
25/094 – Report from the Chair of the Quality Committee for the meetings held on 12 June and 10 July 2025 (agenda item 16)
Dr Healey presented the Chair’s Reports from the Quality Committee meetings held on 12 June and 10 July, taking them as read. She highlighted the need to advise the Board that the domestic abuse, stalking, harassment and honour-based violence assessment (DASH) audit identified low compliance, therefore further detail and review had been requested by the Committee.
She noted the Quality Dashboard review that had taken place and that more detail would be provided at the Committee meeting in September 2025. She also noted the referrals to other Committees as part of the governance structure and processes.
She highlighted that the report regarding patients being classed as absent without leave (AWOL) was being taken through governance discussions to understand the oversight of continuous improvement as this needed to be agreed.
Mrs McRae thanked Dr Healey for the reports.
The Board of Directors received the Chair’s reports from the Quality Committee and noted the matters reported on.
25/095 – Safer Staffing Report (agenda item 17)
Miss Sanderson presented the report taking it as read by the Board. She highlighted the inability to provide registered nurse shift cover on one occasion and that further review of the MHOST data would be undertaken in Q3. She noted that there was a continued high level of vacancies across acute inpatient services but that some vacancies would be filled following recruitment. There was a continued focus on supervision practice and data collected and inputted to improve consistency with compliance figures.
She noted that across the acute female pathway there were higher levels of self-harm and violence and aggression which was linked to the higher levels of bank use, therefore the teams worked consistently above minimum staffing levels.
She highlighted the reduction in vacancies at Red Kite View due to two recruitments and student nurses soon to qualify. She noted that nationally the Trust was engaged in the national programme to improve enhanced care provision through increased observations and the work to develop standards and best practice for implementation and engagement in therapeutic opportunities. She noted that this may lead to increased reporting in restrictive practice due to a change in how it was viewed.
Mr Wright queried the MHOST data collection process and Miss Sanderson responded that it was helpful in some in-patient areas but was linked to the national challenge in that it was the only tool available and not helpful across all areas. She confirmed that there was work ongoing at a national level with mental health services input to review this. She noted it should be considered in line with other tools to provide a more holistic view. Dr Munro acknowledged work undertaken regarding therapeutic observations and the link to costing data as any increase in recording for restrictive practice may change segmentation results, therefore needed to be considered as an unintended consequence.
Miss Wilburn noted that the Specialised Supported Living service was included in several discussions regarding efficiencies and finances, and vacancy levels and patient safety incidents, therefore questioned whether there was a need for further review to understand the detail. Miss Sanderson commented that it was a unique service with limited comparison options, and the tenant group were a unique group of people with varying needs which would impact on some areas, including recruitment. Mrs Forster Adams noted that there had been improvements made with contract arrangements, and the service was subject to frequent review from external agencies. Miss Sanderson added that the peer review process would be included in the next Director of Nursing and Professions report to Board to provide detail and assurance.
Dr Healey noted that six month or annual reporting of data may be more helpful, particularly in some services, and Miss Sanderson acknowledged the point for further consideration of presenting data over a longer period.
Mrs McRae acknowledged the point raised regarding the Specialised Supported Living service and that it would be helpful to see the data in the next Director of Nursing and Professions report. Mr Wright queried whether a recent service visit to the service had taken place. Mrs McRae noted she had visited in the last year however the plan would be reviewed for future service visits and the service would be added if required.
The Board of Directors received the Safer Staffing Report and noted the content.
25/096 – Report from the Medical Director (agenda item 18)
Dr Hosker presented the report taking it as read by the Board. He summarised key areas including a review by the Andrew Sims Centre regarding the admin function to support the wider directorate and changes in models of training. He noted that more information would be provided as the review progressed.
He informed the Board that medical recruitment continued to improve with a reduction in spend on agency doctors, and the Pharmacy Service recovery continued with a focus on culture and the next stage would include governance structures and processes. There was ongoing development of clinical leadership roles, and the Improvement Team were involved in the fourteen organisational priorities and were also reviewing the wider transformation model across the Trust.
Mr Wright asked for clarification regarding the posts listed for AAC panel and Dr Hosker noted that they would go to advert as part of the quarterly process. He added that work was done with the house trainees through the medical leadership team to consider opportunities for individuals.
Miss Wilburn noted that there had been a request from the Mental Health Legislation Committee for more information on the renewal of retentions, and Dr Hosker noted that work was underway with detail expected in September 2025 which would be shared with the Committee.
Mrs McRae noted that the pharmacy recruitment improvement was positive and queried the one year recovery plan progress. Dr Hosker noted that it had started over one year ago, however a listening exercise had been undertaken that generated additional work therefore extended timelines were in place in some areas. He noted he was satisfied with the rate of improvement.
The Board of Directors received and noted the content of the Report from the Medical Director.
25/097 – Guardian of Safe-working Hours Q4 and Annual Report (agenda item 19)
Guardian of Safe-working Hours Q4 and Annual Report (agenda item 19)
Dr Hosker presented the report taking it as read by the Board. He reiterated the role of the Guardian and the mechanisms in place for escalation of concerns via established routes. He noted that the benchmarking results were favourable for the Trust against comparable organisations. He added that there were gaps in the rota periodically which was inevitable due to short term sickness, however mitigation was built in as required.
The Board of Directors received and noted the content of the Guardian of Safe Working Hours Q4 and Annual Report.
25/098 – Report from the Chair of the Workforce Committee for the meeting held on 5 June 2025 (agenda item 20)
In the absence of Mrs Burns Shore the report was taken as read by the Board. Ms Khan highlighted the issue regarding the training space available across the estate, and the outcome of the review of recruitment processes in relation to BAME staff which identified an equitable process. It was therefore hoped that the review of the disciplinary data and process would demonstrate the same level of equity. Mrs Hanwell noted that the estate space issue needed to be considered in the wider discussions around the use of estate across the system.
Mr Skinner noted the job evaluation process with a drive nationally for Boards to be assured regarding processes in place due to grade drift across organisations. He noted that this would allow parity across roles, and the Trust was working through how to provide assurance to the Committee and Board regarding this programme.
The Board of Directors received the Report from the Chair of the Workforce Committee and noted the content.
25/099 – Report from the Director of People and Organisational Development (agenda item 21)
Mr Skinner presented the report taking it as read and highlighted the disappointing minimal change in sickness absence despite the work programmes underway, therefore the focus remained on sickness management action plans, recording of absence and reasonable adjustments implementation when required. He noted that there had been a national increase in complaints to tribunal around reasonable adjustments not being addressed.
He noted that PDR compliance remained stable and acknowledged the work underway. The challenges around staff not attending face to face training were noted and there was a need to review options to drive compliance. He added that there was a focus on recruitment training with all recruiting managers to undertake the appropriate training.
Mr Henry highlighted the benchmarking detail regarding sickness rates with the Trust being in the top three in the region therefore the deeper issues needed to be understood regarding factors for absence. Mr Skinner responded that there was a downward trend in long term absence and an increase in short term so there was a focus on recording and evidencing action taken to address this through the Return to Work process. He added that the Trust was reviewing a system that would support data recording and oversight. Mrs McRae queried if discussion had taken place with other Trusts regarding their position and actions and Mr Skinner responded that there were differences in approaches to sickness management and the Trust focused on wellbeing.
Ms Khan queried if Non-Executive Directors were non-compliant with appraisals, and Mrs McRae confirmed that they were completed but not recorded on the system and this would be addressed. Ms Khan noted that clinical supervision compliance varied across services and Mrs Forster Adams responded that an improvement plan was in place across areas where there was reduced performance.
Mr Wright noted that there had been an internal audit on time and attendance management which found significant assurance which reflected the work that had taken place, and the improvements made.
Mrs McRae thanked Mr Skinner for the report.
The Board received the report from the Director of People and Organisational Development and noted the content.
25/100 – Report from the Chair of the Audit Committee for the meetings held on 17 June and 15 July 2025 (agenda item 22)
Mr Wright presented the Chair’s reports, taking them as read, noting that the Extraordinary committee had taken place prior to the Extraordinary Board of Directors meeting to approve the accounts and reports.
He noted that the July meeting received a number of internal audit reports with several significant assurance results which linked with the private meeting held with the Trust’s internal auditors who commended the Trust’s ability to provide appropriate responses to audits. He highlighted that the Integrated Governance and Risk Management Audit and the Service User Monies Audit had both received limited assurance however the Committee had reviewed the recommendations and were assured with the proposed responses. He added that the Integrated Governance and Risk Management Audit report noted that where risk appetite was referred to there was a need to review the controls associated with each strategic risk to provide evidence for this position which linked to the later agenda item regarding Risk Appetite.
He noted that the sponsorship register was presented with no sponsorships noted and that as part of the medical revalidation process this should be considered to ensure all sponsorships were appropriately captured and noted to ensure the accuracy of submissions.
Mr Henry noted the length of reports provided to the Committee and that the volume and size of reports was increasing which impacted on the time for authors producing reports, therefore there was a need to limit the size of reports. Mrs McRae responded it would be helpful for Chairs of Committees to note issues at the time of the meeting in order to direct authors to specific reports that could be shorted and understand Committee requirements.
Dr Munro noted that the Integrated Governance and Risk Management audit had demonstrated the limitations of the auditor experience in assessing the governance processes in order to get the brief right, therefore this was being further reviewed.
The Board received and noted the content of the Reports from the Chair of the Audit Committee.
25/101 – Board Assurance Framework (agenda item 23)
Dr Munro presented the updated version of the Board Assurance Framework, which demonstrated the current position.
The Board received the Board Assurance Framework and noted the content.
25/102 – Risk Appetite Statement (agenda item 23.1)
Dr Munro presented the report nothing that a risk appetite position had been developed for each strategic risk using the risk matrix and approach from Good Governance Institute. She noted that the proposal had been reviewed at the Executive Risk Management Group with some amendments made following discussion. She noted it was a step change in the Board approach and the recommendation was for the Board to accept the position at the current time, with Committees to consider their specific allocated risks to include the controls and mitigation in place, in line with the risk appetite to balance the potential for innovation whilst also risk tolerance levels.
Dr Healey noted that it was a helpful and clear report however the position was dependent on multiple factors therefore whilst there was a need for a framework there was the need to acknowledge some risks would need to be taken for wider benefit. Dr Munro acknowledged the challenges with agreeing the appetite and it demonstrated the importance of further discussions to understand acceptable failure levels and tolerance.
Mr Wright highlighted that it was important to note that the BAF framework received significant assurance through internal audit, with several reviews showing that there was a good system of control in place. This evidenced that there was a balanced approach to risk in place with a need to focus and refine the list of controls in line with the risk appetite, and consider the level of risk that the Trust was prepared to accept.
The Board agreed to accept the risk appetite position with further discussion to take place at Committee level over coming meetings. Mrs McRae thanked Dr Munro for the report.
The Board received the Risk Appetite Statement and approved the content.
25/103 – Report from the Committees in Common held on 23 July 2025 (agenda item 24)
Mrs McRae referred to the report, taking it as read by the Board. She highlighted the ongoing discussions regarding arrangements as new landscapes progressed, and the prioritisation for mental health support teams in schools in Bradford and Leeds.
Dr Healey queried the target audience for the report and Mrs McRae confirmed that the reports were for Trusts to note as members of the Committee, and if action was required then this would be allocated as appropriate.
The Board received and noted the Report from the Committees in Common held on 23 July 2025.
25/104 – Use of Trust Seal (agenda item 25)
The Board noted that the Trust Seal had not been used since the previous meeting.
25/105 – Any other business (agenda item 26)
There were no additional items of business raised.
25/106 – Resolution to move to a private meeting of the Board of Directors
At the conclusion of business, the Chair closed the public meeting of the Board of Directors at 12:40 and thanked members of the Board and members of the public for attending.
The Chair then resolved that members of the public would be excluded from the meeting having regard to the confidential nature of the business transacted, publicity on which would be prejudicial to the public interest.
Actions outstanding from the public meetings of the Board of Directors
Open Actions
| Log number | Action (including the title of the paper that generated the action) | Person who will complete the action | Meeting to be brought back to / date to be completed by | Update report – comments |
| 24 | Sharing stories – Supporting carers to care with confidence (minute 25/025 – agenda item 2 – March 2025)
It was agreed that a response on updates to the asks for support would be provided to the Board in six months’ time, with Miss Sanderson taking the lead on the action. |
Nichola Sanderson | September 2025 | ONGOING |
| 25 | Report from the Chief Financial Officer (minute 25/040 – agenda item 16 – March 2025)
It was agreed that an update regarding the run rate and justification for staffing levels work would be brought back to the Board in six months time. |
Nichola Sanderson | September 2025 | ONGOING |
| 30 | Declaration of interests for directors and any declared conflicts of interest in respect of the agenda items (minute 25/079 – agenda item 3 – July 2025)
Dr Munro noted that there was need to include her interim role as Chief Executive at Leeds Community Healthcare NHS Trust. |
Corporate Governance Team | Management action | NEW COMPLETE The declarations of interest have been updated to include Dr Munro’s interim role as Chief Executive of Leeds Community Healthcare NHS Trust |
| 31 | Report from the Chief Executive (minute 25/085 – agenda item 8 – July 2025)
It was agreed that the planned autumn Board Development Session would include the 10 Year Plan to consider its implications. |
Clare Edwards | Management action | NEW COMPLETE The NHS 10 Year Plan has been added to the planning for the Board Development Session in October 2025. |
| 32 | Safer Staffing Report (minute 25/095 – agenda item 17 – July 2025)
Mr Wright queried whether a recent service visit to the service had taken place. Mrs McRae noted she had visited in the last year however the plan would be reviewed for future service visits and the service would be added if required. |
Corporate Governance Team | Management action | NEW COMPLETE The Specialised Supported Living Service has been added to the forward plan for service visits. |
Closed actions
| Log number | Action (Including the title of the paper that generated the action) | Person who will complete the action | Meeting to be brought back to / date to be completed by | Update report – comments |
| 28 | 2024 – 2025 Organisational Priorities Quarter 4 Progress Report & 2025 – 2026 New Organisational Priorities (minute 25/060 – agenda item 10 – May 2025)
Mrs McRae commented that there was a need to consider how to align the data to committees and Board and the requirement for the content of the Quality & Culture Dashboard at assurance level, with the proposal to be shared at the June 2025 Board session. |
Chris Hosker | June 2025 (Board Strategic Development Day) | COMPLETE This was discussed at the Board Strategic Discussion day in June 2025. |
| 29 | Report from the Chair of the Workforce Committee for the meeting held on 30 April 2025 (minute 25/066 – agenda item 15 – May 2025)
Discussion took place regarding the data for MSK and stress training and absence, and Mr Skinner agreed to provide the detail on numbers of staff affected to understand the scale of the issue. |
Darren Skinner | Management action | COMPLETE Data has been provided by Mr Skinner (document circulated – item 6.1). |
Actions from Committees for the Board of Directors
None.
Return to agenda
Cover sheet for Chief Executive’s report
- Paper title: Chief Executive’s report
- Date of meeting: 25 September 2025
- Presented by: Dr Sara Munro, Chief Executive Officer
- Prepared by: Dr Sara Munro, Chief Executive Officer
This paper supports the Trust’s strategic objective/s (SO):
- SO1 – We deliver great care that is high quality and improves lives.
- SO2 – We provide a rewarding and supportive place to work.
- SO3 – We use our resources to deliver effective and sustainable services.
This paper relates to the Trust’s strategic risks (SR):
- SR1 – Quality including safety assurance processes
- SR2 – Delivery of the Quality Strategic Plan
- SR3 – Culture and environment for the wellbeing of staff
- SR4 – Financial sustainability
- SR5 – Adequate working and care environments
- SR6 – Digital technologies
- SR7 – Plan and deliver services that meet the health needs of the population we serve.
Executive summary
The purpose of this report is to update and inform the Board of key activities and issues from the Chief Executive.
Recommendation
The Board is asked to note the content of the report.
Chief Executive’s report
The purpose of this report is to update and inform the Board of key activities and issues from the Chief Executive.
1. Our services and our people
Impact of wider societal issues
Over recent months and weeks across the country and locally there has been a rise in protests, marches and actions which have caused people to feel unsafe in their own community. This includes our own staff and service users. Our staff networks along with our EDI lead are creating some spaces for staff to share their experiences and help shape what we can do as an organisation to ensure all our staff feel safe and supported in our communities and how does that extend to the people we support int their own home and in our hospital wards. We have also asked and encouraged teams to discuss in their local team meetings and for anyone with concerns to get support from their line manager in the first instance. We will continue to promote the range of support that is available and support the reporting of hate crime and discrimination.
Service Pressures
The board will note from the COO report that during the past few weeks there has been significant pressure in particular on our acute pathway which has led to an increase in patients needing to be treated out of area. The programme of work to minimise this continues and as we in the period of planning for winter ensuring we have the ability to flex and respond to surges in demand will be important. The board will be asked to sign of our winter plan later in the agenda which is a new requirement of assurance from boards from NHSE. We will also be expected to increase the uptake of flu vaccination rates this winter with targets set at 5% higher than the previous year’s vaccination rates.
Since the last board meeting, we have not had any further periods of industrial action by resident doctors – negotiations continue between the BMA and the government on pay restoration. The BMA is also balloting other groups of doctors for industrial action, and we will keep the board updated on these matters.
Thanks to everyone involved who managed and coordinated our response to the industrial action at the end of July which resulted in minimal disruption and no patient safety incidents in the Trust.
Service Visits
During the summer I was able to visit our forensic services at Newsam, including the forensic outreach team and a visit to ward 6 inpatient adult eating disorder service.
Within our forensic services the progress that has been made in the culture and morale of the staff team was clearly visible when meeting with the now multi-disciplinary leadership team and staff on each of the wards. There have been significant improvements in recruitment across forensic services, and it was great to see the community forensic outreach team is now fully established.
Whilst visiting ward 6 – adult inpatient eating disorder unit – I spent time with service users who gave outstanding feedback for the team on the quality of care and support they have been receiving. They also shared how they can speak directly with the ward manager when they have queries and concerns, and these are always dealt with very promptly. The ward has also been able to recruit successfully to its vacant posts and plan for service development and succession planning.
Staff Engagement
The Thrive and Shine Road shows have come to an end, and I want to thank the staff engagement team and all those who have made it a great success. Feedback form teams has been positive, and it reaffirms our commitment to show our appreciation and recognition for all the work our staff do.
We have also had feedback to the senior leadership team following the Exec led sessions earlier in the summer where we presented our priorities and created space for feedback. The overwhelming feedback is that we should continue to run similar sessions through the autumn though have more time for discussion and feedback. The programme is now being developed and dates agreed.
Finally, we are about to launch the annual staff survey for the NHS. We will be feeding back to staff the impact from last year’s staff survey which we know is not always heard across the organisation – we have a combination of trust wide actions and the local team actions which we know have a direct impact of the experience of people working in the Trust. A communications and engagement campaign will run throughout to encourage as many people to complete the survey as possible.
National Oversight Framework
NHS England has published the 2025/26 NHS Oversight Framework which sets out a revised approach to assessing integrated care boards (ICBs), NHS trusts and foundation trusts for 2025/26. Its goals are to enhance public accountability for performance and improve the identification of providers that require support to improve. It has been developed with the engagement and contributions from the NHS leadership and staff, representative bodies and think tanks, including through two public consultations.
All 205 NHS Trusts have been placed in a segment between 1 (high performing) and 4 (low performing). Entry into a segment 5 will be reserved for the most challenged organisations that require the most support to improve.
Scores are calculated based on performance against agreed metrics across six domains:
- Access to services (elective care, cancer care, urgent and emergency care, mental health care)
- Effectiveness and experience of care
- Patient safety
- People and workforce
- Finance and productivity
- Improving health and reducing inequality (non-scoring) including improving population health, primary prevention, and inequalities
LYPFT has been placed in segment 2, indicating that the “organisation has good performance across most domains” but “specific issues exist”. This reflects good performance across most domains, while acknowledging there are specific areas we continue to improve. Our Trust has been recognised for strong community mental health care experiences and effective crisis team responses, alongside high productivity and value for money. Our main areas of challenge are in sickness absence, and timely discharges from inpatient wards which we are working hard to improve.
NHS Trust Board Provider Self-assessment
As part of the NHS Oversight Framework (NOF), NHS England will assess NHS trusts capability, using this alongside providers’ NOF segments to judge what actions or support are appropriate at each trust. As a key element of this, NHS boards will be asked to assess their organisation’s capability against a range of expectations across 6 areas derived from the insightful provider board, namely:
- strategy, leadership and planning
- quality of care
- people and culture
- access and delivery of services
- productivity and value for money
- financial performance and oversight
These will inform a self-assessment which is intended to strengthen board assurance and help oversight teams take a view of NHS trust capability based on boards’ awareness of the challenges their organisations face and subsequent actions to address them. The purpose of this is to focus trust boards’ attention on a set of key expectations related to their core functions as well as encourage an open culture of no surprises between trusts and oversight teams. NHS England regional teams will then use the assessment and evidence behind it, along with other information, to derive a view of the organisation’s capability.
Where boards already conduct effectiveness reviews, they should consider the degree to which these overlap with this self-assessment. In addition, and to avoid duplication, relevant evidence gathered to support NHS trusts’ annual governance statements can also support the self-assessment.
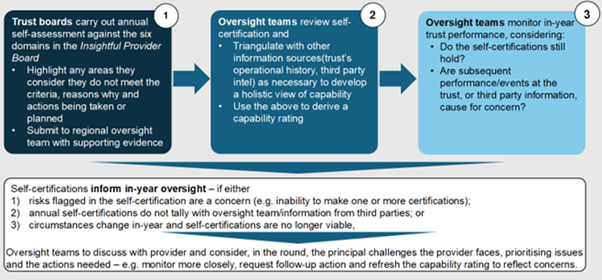
Work is already underway to gather the relevant evidence for the domains outlined in the self-assessment. This is being led and coordinated by the associate director of corporate governance/company secretary working with deputy directors and departmental heads. Once this is completed the board will go through the evidence in detail following which we will then determine our self-assessed ratings to submit to NHSE. We will also agree the ongoing areas for improvement and any support that may be required over the next 12/24 months that can then be included in our annual planning priorities for 2026/27 and our medium-term plan.
Medium Term Planning
NHS Trusts will be expected to develop medium-term plans before the end of this year that will then span 2026-2029. Guidance is being developed, and we expect to understand more about what will be required by October. We will bring further information to the November board meeting assuming the guidance has been published by then.
2. Leeds System Update
Leeds City Ambitions
Following extensive engagement across the city the Leeds City Ambitions have now been finalised and will be launched on the 24th of September at Leeds City College’s Printworks Campus. The ambitions have been developed reflecting on the challenges we face across the city and learning from what has worked so far both locally and nationally. Our Ambitions
HEALTHY: Health and Wellbeing
Leeds will be a healthy and caring city for everyone: where together we create the conditions for healthier lives so people who are the poorest improve their health the fastest, and everyone is supported to thrive from early years to later life.
GROWING: Inclusive Growth
Leeds will be a place where we reduce poverty and inequality by creating growth in our economy that works for everyone, where everyone gets a great education, businesses can find the talent they need to start, innovate and grow and innovate, investment is increasing and together we are delivering an inclusive, healthier and more sustainable future.
THRIVING: Strong Communities
Leeds will be a welcoming, safe and clean city where people have the power to make the changes that are important to them, with cohesive and united neighbourhoods where people are living healthier lives and enjoying the city’s vibrant social, cultural and sporting offer.
RESILIENT: Sustainable City
Leeds will be the UK’s first net zero and nature positive city in the UK, rapidly reducing carbon emissions and restoring nature, a place that supports people and businesses to make increasingly sustainable choices that improve their standard of living while creating a regenerative thriving city.
The Leeds Ambitions provide a strategic framework/roadmap to guide our city’s future and achieve our core mission of tackling poverty and inequality. Our four ambitions are the priorities we’ve set to achieve this mission, grounded in what we’ve learned from our communities and partners. Through working with organisations, communities and people across the city as part of Team Leeds, our four ambitions allow us to align our collective efforts and unlock the added value of our partnerships, ensuring we can accelerate progress and really maximise our impact in the city. Our shared ambition as Team Leeds is for the city to reach its full potential – for everyone living, working, studying or visiting here, it really is the best city. We are a major economic hub, and we believe our growth is strongest when we’re connected. We are building powerful partnerships within the city as well as leaning on our neighbours across West Yorkshire and working with other large cities to drive innovation and ensure a more prosperous future for all.
Leeds Place Provider Review
The review is nearing conclusion with a draft report expected at the end of the month setting out recommendations on how we can strengthen the provider partnership in Leeds to deliver better outcomes for citizens at a neighbourhood level and ensure we have resilient and sustainable models of care for the future – which include greater integration with primary and social care. It will also help us to establish the right governance to enable delegation of functions from the ICB as they work towards implementing the new blueprint for ICB’s.
Dr Wood was SRO for the programme so following his retirement from LTHT I have agreed with the support of partners to take on the SRO role to see through the conclusion on the review.
Leeds Teaching Hospitals Trust
There have been further changes in the leadership arrangements at LTHT. Brendan Brown has now commenced as interim CEO of the Trust for the next 12 months. Brendan was CEO at Calderdale and Huddersfield NHS Trust and CEO lead for WYATT so has very well-established relationships within the city and the ICB. Plans are underway to recruit to executive posts that are due to become vacant in the coming weeks.
National Neighbourhood Health Pilots
The Leeds application to be part of the first wave of the National Neighbourhood Health Implementation Programme (NNHIP) has been successful, along with West Yorkshire neighbours Wakefield and Bradford District and Craven. The programme is a large-scale test, learn and grow change programme. DHSC and NHSE partners will work with 43 local areas across the country to accelerate learning and implementation of neighbourhood health. It will initially focus on targeting adults with or at risk of multiple long-term conditions. Working to ensure that people experience improved health and wellbeing through the support provided at a neighbourhood level.
Through the NNHIP, Leeds will be working over the coming months to develop the programme further. Building on work already started in the city, in line with the Leeds ambitions and the Leeds Health and Wellbeing plan, the programme will be testing:
- Neighbourhood Health Hubs – what processes, culture, assets, and team relationships are needed to operate in an integrated way in existing co-located buildings or virtual hubs.
- Integrated working – understanding what core components are needed to further develop multi-disciplinary teams and co-ordinate care to targeted populations.
- Single and multi-neighbourhood providers – help develop our understanding of how to organise integrated care under future new contractual and financial incentive arrangements, working closely with colleagues in General Practice.
3. Regional and national updates
The Model Region Blueprint for NHS regional teams has now been published. It sets out a high-level mandate for the seven regions and articulates their purpose, core functions and activities. It is anticipated that there will be a Chair and CEO role in each region, but that they will not be independent organisations. They will be part of DHSC in the future.
We know that some functions still being considered, especially workforce, education and training. The Model Region Blueprint also informs the detailed design work that is taking place as part of the DHSC/NHSE Transformation programme over the coming weeks and months.
From the Model Region Blueprint and conversations over the last week, there is now an offer from region to work together with ICBs on this in North East and Yorkshire to inform and influence design of future working arrangements, particularly those functions which we know will move to both region and national teams.
Regions will essentially have three key objectives:
- The first of those objectives is to provide strategic leadership of regional health systems. This means that regions will lead local reform, oversee investment and the reconfiguration of local services; support innovation; and ensure an effective leadership strategy and talent pipeline to get the best from our people. Regions will do this by developing and overseeing implementation of the regional medium-term strategic plan and leading regional implementation of the NHS planning framework. They will support innovation and system development and lead local digital transformation to ensure effective data and analytics capability. Regions will also oversee strategic plans for service and organisational change, set leadership strategy and develop the workforce through training and education.
- The second objective will be to performance manage and oversee local commissioners and providers. This means regions will have holistic oversight of performance in line with national frameworks, ensure Board and leadership capability, as well as identify ‘early warnings’ and manage risk. To achieve this, regions will have oversight of provider and commissioner performance.
- The final objective will be to have a regional approach to improvement, support and intervention. This means regions will support systems and trusts to deliver high quality and sustainable care, develop capability, and address underperformance. This will be achieved by regions providing improvement support, intervening to address challenged performance or providers, and developing commissioning capability and professional leadership.
Last week, NHS England confirmed a number of Chair and CEO roles for ICBs across the country. This was for both clustering ICBs and those which will continue operate on the same footprint. Some Chair roles in ICBs are yet to be appointed. Professor Nadira Mirza will remain the Acting Chair for West Yorkshire until the role is advertised and a national recruitment process takes place. This will be led by NHS England. It has been confirmed that Rob Webster will continue as CEO for NHS West Yorkshire ICB.
4. Reasons to be proud
Baton of Hope
On World suicide awareness day, the Baton of Hope came to Leeds. This is a national campaign aimed at raising awareness of suicide, encouraging more open dialogue to tackle the stigma that exists which prevents people from getting the help they need and ultimately reducing lives lost to suicide. It was founded by a father who lost his son to suicide. The tour through Leeds was organised by Leeds City Council and Touchstone, and we were very proud to be allowed to host the Baton at the Becklin Centre and carry it on to its next stop on the tour. A range of colleagues across the Trust coordinated our contribution which included a project for service users and staff at the Becklin to create an archway of hope through messages using arts. This was led by Arts and Minds and the Recovery college and on the day our Trust Chaplain James held a brief service. Myself along with Steve Taylor (Digital change team) and a father bereaved by suicide carried the Baton in what was a very emotional and powerful experience. The day concluded with a celebration event at the Old Gipton Fire Station. Our videography and communications team are compiling a more detailed article and videos to share across the Trust.
Working Age Liaison Psychiatry Inreach Team
 The Liaison Psychiatry teams at St James’s and Leeds General Infirmary continue to deliver safe, compassionate care for patients with complex mental health needs, even in the most challenging circumstances.
The Liaison Psychiatry teams at St James’s and Leeds General Infirmary continue to deliver safe, compassionate care for patients with complex mental health needs, even in the most challenging circumstances.
They showcase
- Strong collaboration with ward teams ensures holistic care.
- Expertly manage acute mental health risks, including complex discharges.
- Supported eight detained patients while maintaining dignity and safety.
- Led by Cassie, the team promotes best practice and continuity of care.
Acute Liaison Psychiatry Service (ALPS) Team
 The ALPS team has seamlessly integrated research into frontline care, delivering tailored therapy to individuals presenting after repeated self-harm, while maintaining a 24-hour service.
The ALPS team has seamlessly integrated research into frontline care, delivering tailored therapy to individuals presenting after repeated self-harm, while maintaining a 24-hour service.
They achieved
- Delivered the Fresh Start trial with Research and Development.
- Trained clinicians in specialised therapy approaches.
- Recruited 70 participants, highest across all NHS trusts.
- Provided therapy to 36 individuals with clarity and compassion.
Trevor – Individual of the Month
 Trevor, Clinical Team Manager at the Becklin Centre, showed exceptional leadership during a security incident, ensuring safety and calm throughout.
Trevor, Clinical Team Manager at the Becklin Centre, showed exceptional leadership during a security incident, ensuring safety and calm throughout.
Leadership in Action
- Led with clarity and calm during a security incident.
- Provided tailored support to lone workers.
- Reassured staff and service users throughout the event.
- Maintained a safe, supportive environment under pressure.
Sara’s Spotlight Award – Wan
Wan’s creativity, compassion, and leadership have made a lasting impact on the UPLIFT project, supporting refugee and asylum-seeking women through perinatal mental health challenges.
- Guided the UPLIFT project with insight and dedication.
- Inspired meaningful change for vulnerable communities.
- Brought the project to life through Me & Ma social media content.
- Celebrated as Research Hero of the Month – August 2025.
Research Heros – SPACES Trial Champions: Luke, Efemena, and John
 Delivered 18-week physical activity programme
Delivered 18-week physical activity programme- Balanced research with core Trust roles
- Built confidence, connection & wellbeing
- Co-produced with service users
- Positive feedback from participants
- Inspired future involvement in research
Dr Sara Munro
Chief Executive Officer
18 September 2025
Cover sheet for Chief Financial Officer (CFO) Finance Report
- Paper title: CFO Finance Report
- Date of meeting: 25 September 2025
- Presented by: Dawn Hanwell, Chief Financial Officer and Deputy Chief Executive
- Prepared by: Jonathan Saxton, Deputy Director of Finance
This paper supports the Trust’s strategic objective/s (SO):
- SO3 – We use our resources to deliver effective and sustainable services.
This paper relates to the Trust’s strategic risks (SR):
- SR4 – Financial sustainability
Executive summary
The Trust is on plan in month 5 but only due to one off non-recurrent means, this demonstrates the importance of the expedient delivering of the efficiency programme. The capital plan is currently behind plan but expected to achieve plan by the year end.
The system is behind revenue plan YTD due to the impact of industrial action, pay overspends and slippage on delivery of waste reduction/efficiencies but still forecast a breakeven position by year end.
There is to be an additional productivity metric within the Finance and Productivity domain in the National Oversight Framework. Although the calculation has been shared with the Trust, the exact costs and activity that will go into calculating the score is yet to be ascertained. The Trust has completed it’s first submission in the deconstruction of income block contract exercise. Through undertaking the exercise, it has shown that there is much improvement to be made in Mental Health costing and activity information. Both the new NOF metric and the Deconstructing the Block exercise have highlighted the importance of recording and reporting activity data.
Work has begun on the medium term planning process, including identifying the start point of “underlying position”. The timescales for the planning process will be challenging.
Do the recommendations in this paper have any impact upon the requirements of the protected groups identified by the Equality Act? No
Recommendation
The Board is asked to:
- Note the Trust revenue & capital positions for 2025/26.
- Note the system position.
- Note the importance of recording and reporting accurate activity data
CFO Finance Report
1 – Introduction
This report provides an overview of the financial position at the end of month 5, 2025/26 financial year. It also includes some other relevant updates and information.
2 – Income and Expenditure Performance 2025/26
The overall summary reported position to NHSE against the Trust plan is shown in table below. This reflects a position broadly on plan overall (surplus of £48k).
Income and expenditure plan position for month 3
| Category | Plan Annual (£’000) | Plan YTD (£’000) | Actual YTD (£’000) | Variance YTD (£’000) |
| Patient Care Income | 235,819 | 101,757 | 101,870 | 113 |
| Other Income | 37,634 | 12,328 | 13,362 | 1,034 |
| Total Income | 273,453 | 114,085 | 115,232 | 1,147 |
| Pay Expenditure | (200,366) | (84,033) | (82,573) | 1,460 |
| Non Pay Expenditure | (68,406) | (27,934) | (30,607) | (2,673) |
| Total Expenditure | (268,772) | (111,967) | (113,180) | (1,213) |
| Surplus / Deficit | 4,681 | 2,118 | 2,052 | (66) |
| Adjustments for NHSE Reporting | (4,681) | (2,118) | (2,004) | 114 |
| Adjusted Position | 0 | 0 | 48 | 48 |
The key items of note overall in the position are:
- Bank expenditure remains at an average of £1.4m per month and is £605k above plan year to date. This is largely driven by increased evening and weekend usage of bank working.
- Agency expenditure has reduced in year and is £1.1m under plan year to date. The majority (89%) of agency is related to medical staff.
- Substantive pay expenditure is also £954k under plan, largely attributable to management of recruitment, linked to assessing recurrent cost savings.
- Against the in-year trajectory Adult Acute Out of area placement (OAP) spend is £2.1m cumulatively overspend year to date. This is concerning given the reducing trajectory for the year.
- Overall corporate departments, doctors in training and pharmacy have broadly started the year along the same pattern as they exited the prior year, with significant vacancies and underspend.
- Non-recurrent benefits such as technical flexibilities, interest Receivable above plan and the delay in recruiting to the additional Perinatal ward are supporting the position, this is in the region of £3.2m.
3 – Efficiency Programme
3.1 – Run Rate efficiency
The efficiency programme target is to deliver in year run-rate savings of £18.5m. This is based on our system plan, which reflects run rate movements year on year (not recurrent internal budget).
Year to date £6.9m of run-rate reductions have been achieved compared to the year to date (YTD) target of £7m, £134k behind target as shown below:
| Schemes | Recurrent / Non-recurrent | Risk | YTD Plan (£000) | YTD Actual (£000) | YTD Variance (£000) |
| Interest receivable | Non-recurrent | Low | 1,565 | 2,138 | 573 |
| CPC Gainshare | Recurrent | Low | 210 | 208 | (2) |
| Technical Flexibility | Non-recurrent | Low | 1,387 | 1,374 | (13) |
| Reducing Agency 30% | Recurrent | Low | 500 | 1,576 | 1,076 |
| Reducing bank 10% | Recurrent | Medium | 298 | 108 | (190) |
| OAPs improvement | Recurrent | High | 1,375 | 0 | (1,375) |
| Non-Pay savings | Recurrent | Low | 415 | 184 | (231) |
| unidentified | Recurrent | Medium | 1,250 | 0 | (1,250) |
| Overtime reduction | Recurrent | Low | 0 | 199 | 199 |
| Additional Income Agreed | Recurrent | Low | 0 | 246 | 246 |
| Non-recurrent income | Non-recurrent | Low | 0 | 748 | 748 |
| Reducing Pay (Recurrent) | Recurrent | Low | 0 | 85 | 85 |
| Reducing pay (non recurrent) | Non-recurrent | Low | 0 | 0 | 0 |
| Total | – | – | 7,000 | 6,866 | (134) |
| – | – | – | – | – | – |
| – | Recurrent | – | 4,048 | 2,607 | (1,441) |
| – | Non-recurrent | – | 2,952 | 4,260 | 1,308 |
| – | – | 7,000 | 6,866 | (134) |
Two major recurrent schemes, OAPs expenditure improvement and reducing Bank expenditure by 10% are significantly behind plan. The position has been predominantly mitigated by non-recurrent schemes including additional non-recurrent income and interest receivable. It is important to note the balance between recurrent and non-recurrent delivery as whilst overall the position appears reasonable, the impact of under delivery on recurrent schemes will impact the exit run rate for the year and impact on the underlying assessment of financial performance. The level of reliance on non-recurrent measures is not a sustainable position for the organisation and the major run rate pressures must be addressed on a recurrent basis, through the efficiency workstreams.
3.2 – Budget efficiency
The Trust’s recurrent internal budgets identified a recurrent £14.5m budget saving programme (recurrent CIP). This is based on allocated budgets not run rate profiles. It is a target figure to balance budgets. assuming every service and department is operating from their opening base budget position, not what is being spent (run rate). In August the first Quality Impact Assessment (QIA) panel was held where a 49 schemes were agreed to be progressed, this resulted in £6.2m of schemes being transacted in the month. An additional QIA panel is due to be held in September where it is expected further schemes will be agreed and transacted. The current position is below:
| Div/Dept | 25/26 target | 25/26 target | Awaiting QIA today | % of target achieved |
| CFO | 2,000 | 1,653 | – | 83% |
| POD | 650 | – | 34 | 5% |
| Nursing | 600 | – | 367 | 61% |
| Care Services | 9,700 | 3,140 | 114 | 24% |
| Medical | 850 | – | 136 | 16% |
| CEO | 200 | 133 | – | 67% |
| COO | 50 | 50 | – | 100% |
| Reserves | 450 | 1,206 | 258 | 325% |
| Total | 14,500 | 6,182 | 909 | 49% |
To date £6.2m of schemes have been transacted, it is expected a further £0.9m will be transacted in September, this would leave a residual target of £7.4m (51%) still to be achieved.
4 – Capital Expenditure
The capital position is detailed in Appendix A. Cumulative year to date capital expenditure is £3.6m at M5 against a plan of £8.7m. The YTD plan includes £4.5m of PDC capital expenditure for Parkside Lodge (actual £730k at M5), which is now forecast later this financial year. Expenditure includes network infrastructure £0.24m phased later in year in the plan.
Providers plan for capital expenditure at 105% of capital allocations, with an acknowledgement that they must operate within the allocation (100%) in year. To facilitate this, LYPFT’s 2025/26 capital plan includes £2m (phased later in year) on behalf of all providers within the ICS.
5 – National Oversight Framework (NOF) Update
Currently there are 3 metrics that form the Finance and Performance domain within the NOF, as shown below:
| Domain | Metric |
| 5. Finance and Productivity | • Planned surplus/deficit, • Variance year-to-date vs. financial plan, • Relative difference in costs (specific productivity measure for MH) |
Productivity is a measure of outputs relative to inputs. In healthcare, it can be summarised as the amount of activity the NHS delivers (appointments, scans, etc) for the inputs used in delivering that activity (on staff, consumables, buildings, etc). Broadly speaking, increasing the volume of outputs by more than the volume of inputs leads to productivity growth, or maintaining output but with fewer inputs.
Improving productivity is a key priority for the NHS, as part of the focus on delivering value-based healthcare. This is made clear in the 10 Year Health Plan, which states improving productivity as the central goal for the reforms set out. A monthly estimate of NHS trust productivity is being published from September 2025 and it is anticipated that this score will be used as one of the NOF metrics in Q3. The formula for calculating implied productivity is shown below:
Productivity Growth (%) = 1 + cost weighted activity growth / 1 + real terms cost growth -1
NHSE have sent the YTD M2 productivity growth to organisations, the Trust score is -29.7%. The score is an outlier nationally and as a result, NHSE have contacted the Trust to ascertain the rationale. In M2 there was an error in submitting Trust activity data to NHSE which led to the adverse score. We have tried to contact NHSE to explain the Trust score and further identify exactly how the score is exactly derived, at the time of writing the report we are yet to hear a response. As this metric will form part of the NOF starting later this financial year, it highlights how important activity recording and reporting will become for the Trust.
6 – Medium Term Planning Framework
The high-level planning framework has been published with more detailed guidance and templates to follow in October. The indicative timeline will be challenging with an expectation that plans will be finalised at provider level in December. In the context of all the national and regional changes, individual providers will now be required to produce organisational level plan narrative (for 5 years) alongside 1-to-3-year financial plan. There will no longer be a single ICB level plan.
From a finance specific perspective, we have been required to commence 2 pieces of work as the foundation for the medium-term plans. These are “Deconstructing the Block” income and assessing the underlying financial position. Each is noted below.
6.1 Deconstructing the Block
The 10-year health plan set out the need to deconstruct block contracts predominantly to support the move to neighbourhood health services, and ultimately to change payment mechanisms and financial incentives. There is also a recognition of the need to redefine the links between productivity/efficiency and income which have been “lost” due to the payment arrangements introduced during COVID. Being able to quantify the extent to which providers are currently over or under paid in their existing contracts by ICBs when compared to an activity x price basis is an essential first step in deconstructing block payments. The NHS cannot move to new payment mechanisms without understanding the baseline financial position.
The exercise is a comparison of 2025/26 contracts values compared to 2024/25 outturn activity priced at an adjusted national average cost. The MH national average costs are based on 2023/24 national cost data deflated by 29% to strip out unit cost growth between 2019/20 and 2023/24 then uplifted by 19.2% for the compounded Cost Uplift Factor (CUF) between 2019/20 and 2025/26. This calculation results in a reduction a 7.58% of the 2023/24 national average. In mental health it is recognised that the availability of robust activity and cost data will limit the analyses that can be done. Given the scale of the issues raised by the sector current expectation is that there will be no financial impact from this exercise enacted in 2026/27 for mental health trusts. Issues with the 2023/24 National Cost Collection have previously been highlighted to the committee.
The ICB submission deadline was 12 September, the ICB then collated all submissions ready for the submission to NHSE. This exercise does not include services commissioned through provider collaboratives where LYPFT is not the lead provider (i.e. forensic and York CYP services). The Trust submission shows a gap in contract income against contracted services of c. £26m (i.e. presentational “over payment”). High level benchmarking with similar MH Trusts identifies a consistent level of significant gaps. Nationally it is fully acknowledged that data quality in the Mental health and community sector is a key barrier. The next steps in this exercise are to form more detailed working groups to refine the information going forwards. There is no clarity at this stage on what the potential impact will be on contract income approaches for future years, but there will be no immediate impacts.
6.2 Underlying Position
NHSE recognise the underlying financial position as defining the true, sustainable financial health of an organisation, once the impact of one-off, temporary, or exceptional items are removed from the reported figures. It is based purely on the actual expenditure and income of the Trust (run rate), not budget.
The board need to understand the underlying position because it reveals the real financial sustainability of the organisation, highlights recurring gaps between income and expenditure, supports better strategic decision-making about cost control, investments, and transformation plans and informs discussions with regulators about future funding.
An exercise has been undertaken to identify the underlying position, and this forms the starting point for the medium-term financial plan. Our assessment demonstrates an underlying position of £4.3m deficit, which has been discusses in detailed at the Finance and Performance Committee. This is largely driven by the slippage in delivering solid recurrent savings run rate savings as noted above.
7 – System Financial Position
7.1 System M5 Revenue Position
The month 5 year-to-date position for the ICS was an actual £36.1m deficit against a planned £26.8m deficit; a shortfall/adverse variance against plan of £9.3m. The month 5 adverse variance of £9.3m has improved from the adverse variance at month 4 of £11.9m, an improvement of £2.6m. The improvement in month is driven by a reduction in costs associated with prescribing and an underspend on pharmacy contracts within the ICB. The key drivers of the YTD adverse variance continue to be industrial action, pay overspends and slippage on delivery of waste reduction/efficiencies, part offset by underspends in other areas. The ICS continues to forecast a balanced plan to NHSE at Month 5 (based on receipt of £49.2m deficit support funding).
To ensure systems continue to plan to deliver revenue positions, further guidance has been issued in year on “Strengthening Financial Management”. Largely this is an update on all the measures introduced last year. However, one new area of guidance relates to cash management arrangements and how systems are expected to cooperate to manage day to day cash challenges across Trusts. A paper discussing the potential impact for the Trust has been discussed in the Finance and Performance Committee.
7.2 The System M5 Capital Position
Year to date there is a £27.7m underspend against the system operational and IFRS16 capital plans and a £25.5m underspend against the National PDC Capital plans. It is expected that all capital plans are delivered by the end of the financial year. Plans include an additional 5% ‘over programme’ to reflect potential slippage in the year, an additional £8.8m. Providers are aware the 5% over programme plans can only be spent if there is capital slippage.
8 – Conclusion
The Trust is on plan in month 5 but only due to one off non-recurrent means, this demonstrates the importance of the expedient delivering of the efficiency programme. The capital plan is currently behind plan but expected to achieve plan by the year end.
The system is behind revenue plan YTD due to the impact of industrial action, pay overspends and slippage on delivery of waste reduction/efficiencies but still forecast a breakeven position by year end.
There is to be an additional productivity metric within the Finance and Productivity domain in the National Oversight Framework. Although the calculation has been shared with the Trust, the exact costs and activity that will go into calculating the score is yet to be ascertained. The Trust has completed it’s first submission in the deconstruction of income block contract exercise. Through undertaking the exercise, it has shown that there is much improvement to be made in Mental Health costing and activity information. Both the new NOF metric and the Deconstructing the Block exercise have highlighted the importance of recording and reporting activity data.
Work has begun on the medium term planning process, including identifying the start point of “underlying position”. The timescales for the planning process will be challenging.
9 – Recommendation
The Board is asked to:
- Note the Trust revenue and capital positions for 2025/26.
- Note the system position.
- Note the importance of recording and reporting accurate activity data.
Jonathan Saxton
Deputy Director of Finance
18 September 2025
Cover sheet for Report of the Chief Operating Officer
- Paper title: Report of the Chief Operating Officer
- Date of meeting: 25 September 2025
- Presented by: Joanna Forster Adams, Chief Operating Officer
- Prepared by: Members of the Care Services’ Senior Operational Leadership Team
This paper supports the Trust’s strategic objective/s (SO):
- SO1 – We deliver great care that is high quality and improves lives.
- SO2 – We provide a rewarding and supportive place to work.
- SO3 – We use our resources to deliver effective and sustainable services.
This paper relates to the Trust’s strategic risks (SR):
- SR1 – Quality including safety assurance processes
- SR2 – Delivery of the Quality Strategic Plan
- SR4 – Financial sustainability
- SR5 – Adequate working and care environments
- SR7 – Plan and deliver services that meet the health needs of the population we serve.
Executive summary
This report is presented to the September Board of Directors’ meeting to set out the key management, development, and delivery issues across LYPFT Care Services and to highlight any potential impact for the population we serve. It is derived from work with operational, clinical and quality colleagues, where information and intelligence is used alongside experience, to establish where we should prioritise our efforts for improvement (and recovery where necessary). Our established arrangements for operational and clinical governance enable us to highlight key areas for the attention of the Board. This report has been presented and discussed in the Finance and Performance Committee.
Do the recommendations in this paper have any impact upon the requirements of the protected groups identified by the Equality Act? No
Recommendation
The Board of Directors is asked to be assured of the work being undertaken to deliver our care services and to manage the range of challenges and issues outlined in this report.
Report of the Chief Operating Officer
1 – Introduction
This report sets out the key management, development, and delivery issues across LYPFT Care Services. It aims to summarise and highlight the most significant service delivery issues we are managing.
Primarily, the main areas of concern are set out in the “Alert” section of the Service Delivery and Key Performance Escalations section of this report (Section 2.1 below). However, as a very high-level summary the most concerning issues include:
- Acute flow and Out of Area Placements
- Physical health assessments on inpatient wards and in the Aspire Early Intervention in Psychosis Service
- Enteral feed and oral nutrition support (ONS) supply.
2 – Service Delivery and Key Performance Escalations
2.1 Alert
This section sets out the key areas of concern for care services that have been identified through our governance arrangements. These updates relate to the areas where services face most challenge and where risks are highest.
2.1.1 – Acute Flow and Out of Area Placements
2.1.1.1 – Current Position
Acute Flow, and consequently the number of Out of Area Placements has deteriorated significantly resulting in quality, performance and financial risks. The position is as follows:
Graph 1
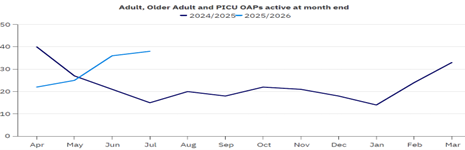
Our planned trajectory and performance against it is:
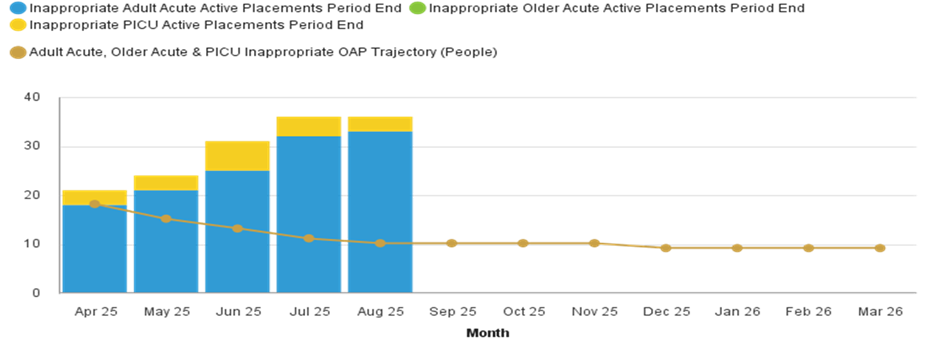
We are off target in reducing inappropriate OAPs as actual placement numbers continue to exceed the planned reduction trajectory. During July and August 2025, a total of 37 new placements were commenced and those patients received inpatient care in services located outside of Leeds.
Whilst placements were primarily concentrated in County Durham and Bradford, patients were also placed in various locations across England. This was largely due to limited bed availability within the private sector, which constrained local placement options.
Placement decisions are based on clinical urgency and bed availability, rather than proximity and at the end of August, the furthest placement South of Leeds was in Nottingham.

2.1.1.2 – Demand
Over the 12-month reporting period, bed management referrals have shown fluctuating demand, with notable peaks in February, June and July 2025.
Graph 3
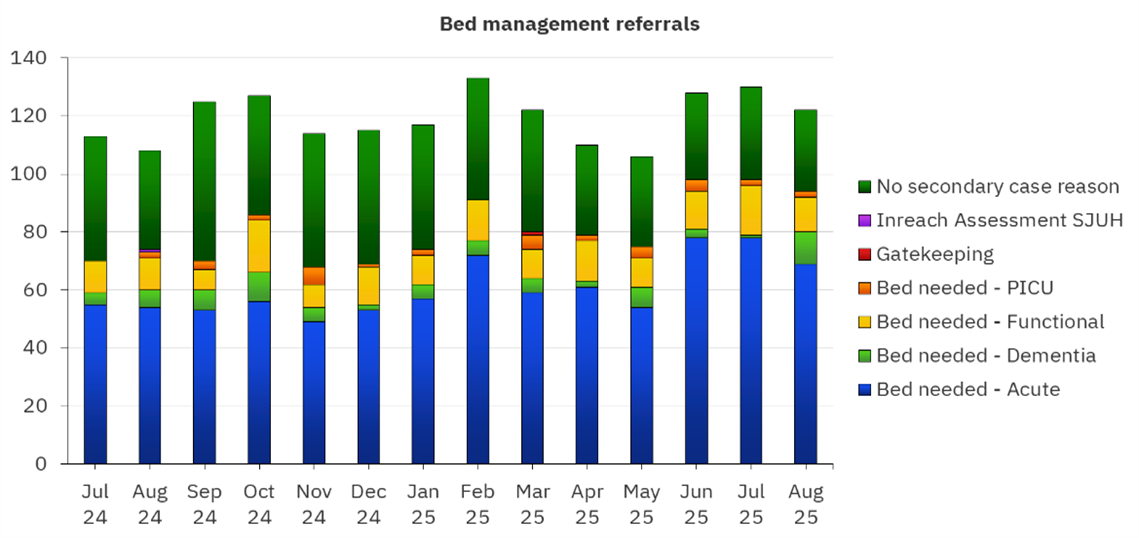
Key issues affecting this include:
The closure of the Oasis Crisis House on 4 July 2025 which resulted in a reduction of 5 crisis beds within the Leeds system. Since that time, 25 patients who may have otherwise been supported through crisis care have been admitted to our acute inpatient wards.
This has placed additional demand for acute inpatient admission, reducing alternatives to admission options and contributing to slower patient flow. Crisis beds typically serve as a diversion from hospital admission or as a step-down option, and their absence has led to:
- Increased demand for acute beds, which are already under pressure
- Reduced capacity for timely admissions, particularly for patients in crisis who could have been managed in a less restrictive setting
- Potential delays in discharge, as patients who might have transitioned to crisis support remain in acute care longer.
The reopening of Oasis has been delayed because of additional structural work required. We are awaiting an update on when this is likely to be completed.
2.1.1.3 – Delayed Discharges
In August, there were a total of 484 delayed bed days across the acute inpatient wards. Notably, 51% (248 days) of these delays were attributed to housing-related issues, making this the single largest contributing factor. It should be noted that delayed bed days peaked in March when the Trust recorded 855 delayed bed days, with 55% linked to housing delays. However, since then, there has been a steady decline, and this downward trend suggests that efforts to reduce delays may be having a positive impact.
Graph 4 below shows the breadth of reasons for delays across the system.

2.1.1.4 – Housing
Housing delays can be broken down further into 5 categories:
- Awaiting supported accommodation
- Awaiting temporary accommodation from the Local Authority
- Awaiting rented housing via council housing waiting list
- Awaiting private rented accommodation
- Patient not eligible for funded care or support.

Graph 5 above shows that supported accommodation has remained the leading cause of housing-related delays this year. However, a positive shift has happened in the sector with improvements since the peak in February 2025. This is due to sustained work led by colleagues in the ICB aimed at increasing the market for this supported accommodation. This positive work needs to be sustained despite the changes happening at an ICB and NHSE level in the next few months. Additionally, we are seeing a growing number of individuals who do not meet the eligibility criteria for funded care or treatment. This group accounted for 195 delayed bed days during the period, adding further complexity to discharge planning. Additionally, August 2025 saw a rise in delays linked to individuals awaiting temporary accommodation from the Local Authority, contributing a further 40 delayed bed days.
To address housing-related discharge barriers in acute inpatient wards and the Transitional Housing Units, where many of our patients move onto, Leeds City Council has appointed two Mental Health Housing Officers (1 permanent and 1 on a 12 months fixed term contract), jointly funded by the ICB and LYPFT. Their role is focused on supporting timely discharge for patients facing accommodation challenges, particularly by reducing delays in our inpatient wards and the Transitional Housing Units, where bottlenecks have impacted system flow. This is a proactive step towards improving patient throughput and reducing pressure on inpatient capacity.
Safe and timely discharges have been a key workstream of the Improving Patient Flow Programme which is now incorporated into the Improving Inpatient Quality Programme. This workstream is critical to reducing Length of Stay (LoS), ensuring patients are discharged promptly once clinically ready, without compromising safety or continuity of care.
Reducing LoS is essential to meeting NHS England Operational Planning requirements and achieving our agreed trajectory. To support this, we are working closely with Local Authority and ICB colleagues to expedite housing and placement solutions and address systemic delays.
Our performance against the planned trajectory is:
Graph 6

The average LoS for adult acute and older adult inpatients has shown gradual improvement from April to August 2025, aligning with the projected trajectory and supporting progress toward NHS England planning targets.
However, this headline measure masks underlying pressures. A snapshot at the end of August showed that 58 out of 109 patients (53%) in acute wards had a LoS exceeding 60 days, highlighting a significant cohort of long-stay patients. As previously highlighted, these extended stays are often linked to complex discharge barriers, including housing, specialist placement delays and Ministry of Justice restrictions.
To address these challenges, weekly multi-agency discharge meetings are held to ensure a collaborative approach to resolving delays.
Tracking change in the number of patients clinically ready for discharge (CRfD) has become more challenging due to a change in classification methodology in early 2024, making current data non-comparable with previous reporting periods.
A current snapshot of the data shows:
- 5% of patients in acute beds are CRfD, equating to 20 out of 109 beds
- Of those with LoS greater than 60 days (in acute wards), only 31% are clinically ready for discharge
- In PICU, there are currently no patients classified as CRfD; however, 2 patients are awaiting specialist forensic placements, contributing to delayed transfers of care.
2.1.1.5 – Immediate Response to Increased Acute inpatient pressures
In response to the recent surge in acute inpatient pressures, a series of immediate actions has been implemented beyond existing programme work. Daily Capacity and Flow meetings have been embedded to support rapid decision-making and resource deployment, alongside enhanced bed management protocols and daily OPEL reporting to system partners.
To accelerate discharge and alleviate acute inpatient pressures, weekly ward-level capacity meetings and multi-agency discharge meetings have continued, supported by strengthened liaison with Adult Social Care to expedite care package arrangements where appropriate. In addition, regular reviews have been introduced for patients who are not classified as CRfD but have remained on an acute ward for over 60 days, to identify barriers to progression and explore alternative pathways.
2.1.1.6 – Improving Patient Flow Programme
Quality Risks
The issue of how we oversee the quality of care in our spot purchased Out of Area Placements has been subject to active review at the Quality Committee. In April 2025, the Head of Operations for Acute Services outlined in a paper to the Committee how we support in-reach and oversee the quality of individual placements. These arrangements are active and the care and treatment of Leeds patients in out of area inpatient facilities is overseen by the Capacity and Flow Team, supported by relevant community services. Currently the resources we have in this team are meeting demand.
Financial Risks
At the end of Month 5, the Acute and PICU Out of Area Placements budget was significantly overspent, with a £2.1 million variance against the phased annual budget of £3.5 million. The budget is aligned to expected activity trajectories rather than evenly distributed across the year, but current expenditure indicates sustained and higher-than-anticipated demand. Forecasting is routine and incorporated into our financial planning and management arrangements.
2.1.2 – Physical health assessment on inpatient wards and in Aspire
Achieving the standard of physical health assessment is important to the health and health improvement of our service users and it links directly to the ambitions of our Improving Health Equity priorities.
Our compliance with this key performance indicator has been declining, and in July 2025 the COO reported that recovery actions were being established and led within services, and our current performance is reported as follows (see Graph 7).
Graph 7

Our Acute and Forensic Services are not achieving the standard and require improvement actions. In summary the reasons for this include:
- Variation in completion by profession (see Graph 8 below)
- A decline in the completion of the medical assessment during the period of changeover for Resident Doctors
- Incorrect assessment tools being used and completed in Forensic Services.
Actions are being taken across services; mainly focused in the Acute and Forensic services to address these issues. Importantly the development of physical health improvement plans is underway in our Acute and Forensic Services, and this will be part of our health improvement work across the directorate.
The Forensic Service has also developed these plans as a requirement for the West Yorkshire Provider Collaborative for the service at the Newsam Centre in Leeds. These plans will also be implemented at Clifton House in York.
This should link to the issues some service users face when reluctant to participate in or to be assessed. How we approach this in practice should be central to physical health improvement plans for service users, linked directly to the known poor outcomes for patients with serious and enduring mental health problems.
Compliance with the measure will be monitored and managed through our Care Services Performance Group which includes leads from all services.
Graph 8
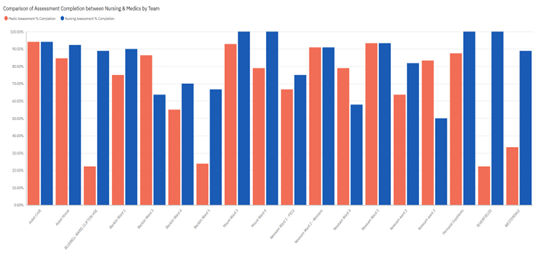
Note: This graph shows an average completion in each area over a 12-month period and may not reflect the current position.
Aspire is also taking significant steps to improve their compliance with this KPI (see Graph 9). One of the challenges that Aspire has, like that of the inpatient wards, is when service users choose to decline to engage in the assessment. Whilst the assessment completion requirements are the same as the inpatient areas, we are exploring how the logic we use for our KPI differs from what is measured in the National Audit of Psychosis (NCAP) audit, which allows for the recording of declined assessments. Whilst this is still being explored, we will continue to strive to improve the recording of these assessments.
A Service Development Improvement Plan is in place with ASPIRE to support increased performance. Alongside the focused work regarding the logic, one member of staff has been deployed to focus on improving physical health check compliance. In addition, ASPIRE has secured a research practitioner who has been funded until 2028 and who is offering additional capacity to complete the checks.
Graph 9

2.1.3 – Enteral Feed and Oral Nutrition Support (ONS) Supply
The risks relating to the disruption of supply of our enteral feeds primarily affects our Learning Disability service users with our staff working hard to mitigate this. Currently other teams within LYPFT who use enteral feeds report no ongoing significant issues.
While Nutricia stocks seem to have improved to some extent, this is variable, and improvements are not always sustained. There is ongoing work to support service users and carers to revert to original feeds where possible and ensure that correct feed regimes are being followed.
NHS England reports that Nutricia’s new factory is moving forward, and they are seeing noticeable progress resulting in demonstrable improvements on several key metrics around impact of product availability, call responses and backorder issues.
The Community Learning Disability Dietetics Team was hoping to step down the duty system which is being used to manage these difficulties; however, over the past two weeks they have again seen an increase in out-of-stock notifications related to specific bottle sizes of some of the core feeds.
Where specific bottle sizes were not available, Nutricia staff have, in the past, been sending out alternative bottle sizes without contacting the dietitian. However, due to concerns being raised about Nutricia providing advice to patients with regard to the different bottle sizes, and the potential for this to lead to possible patient safety issues, an agreement was made that Nutricia staff would contact dietitians for any changes in bottle sizes instead of ordering these automatically. This has led to an increase in dietetic workload.
There are also concerns that Nutricia has changed some of their internal processes related to the out-of-stock notifications, so we have requested the up-to-date process from Nutricia which we should be receiving soon.
The plan agreed to mitigate issues with enteral feed supply is as follows:
- Continue with the duty system due to an increase in notifications and low levels of staffing
- The lead dietician to liaise with other lead dietitians in Leeds as to how they are managing the current increase in out of stocks related to bottle sizes
- Continue to pursue the engagement of a locum and explore any limited options for redeployment / mutual aid across the organisation
- Request and receive the back-order process from Nutricia
- On duty days, the team is to continue working through the ‘resolved issue’ list and check in on those who have been on alternative feed regimes to ensure they are back on their usual feed.
A Tactical Group continues to meet on a fortnightly basis to gather intelligence, assess risks and identify options and contingencies.
2.2 – Advise
2.2.1 – Adult Acute: Crisis Resolution Response Performance
Our performance against the 4-hour response target is reported as 58% in August which is a deterioration of 11% against performance as reported in the July COO Board report. The number of people who require a very urgent response continues to be low at 28 in August. This means that any variation in timeliness and reported non-achievement of the standard can skew the position. We are working to understand why we have seen a marked decrease in urgent referrals and include this in our work to provide optimally responsive crisis services.
As previously reported, we are working with the CareDirector team to look at how performance can be more accurately reported as there were, in fact, 5 breaches in the period which should not have occurred. Dashboards are being worked on with an expected roll out at the end of September, beginning of October.
2.2.2 – Emergency Department (ED) waits for mental health assessment
ALPS referrals increased in August reaching 343 as shown in Graph 10 below, which is higher than the same time last year (324 referrals in August 2024). This was also the highest referral rate since March 2024 where 344 were received.
Graph 10
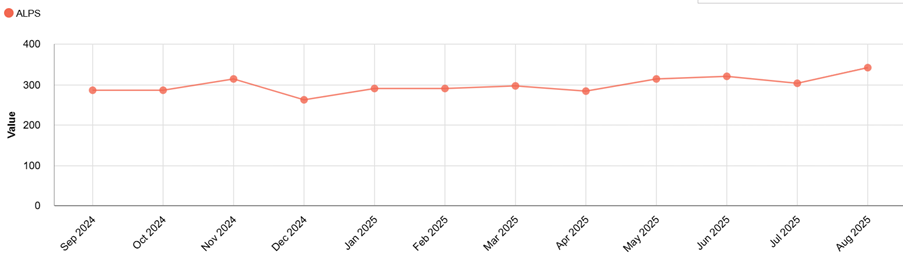
As part of the Reducing Mental Health ED Attendances and Delays Project (part of our strategic priorities programme), we are undertaking a comprehensive review of ALPS activity data. A key focus of this programme is the development of a dataset to identify which of the service users who have been referred to ALPS have had prior engagement with LYPFT teams. This will help us explore whether earlier crisis interventions might have been feasible, and what steps we need to take in our care pathways to help prevent ED attendance.
In preparation for winter, we also plan to audit care plans to assess the extent to which service users are being advised to attend the ED during a crisis. This will support our efforts to anticipate referral patterns and identify opportunities to redirect individuals to more appropriate crisis pathways, thereby reducing pressure on emergency services.
With regard to the ALPS one-hour response, this continues to present a challenge with our response rate in August being at 63% (see Graph 11 below).
Graph 11

To address this, we have implemented a targeted local action plan aimed at driving improvements in performance. We have responded to staffing gaps caused by vacancies by recently deploying colleagues from other teams within the service, which has provided some mitigation. As part of our efforts to strengthen capacity within ALPS, two new staff members have recently joined the team which is helping to alleviate existing workforce pressures.
Looking ahead, we plan to undertake a broader review of staffing establishments within the scope of the Reducing Mental Health ED Attendances and Delays Project. This will enable us to better anticipate demand, identify potential gaps, and implement more sustainable workforce solutions to support timely crisis responses.
2.2.3 – Red Kite View Management
We are currently facing leadership staffing challenges within Red Kite View on both Skylark and Lapwing wards. Team Managers for these wards will be leaving their posts in September; one permanently and one due to maternity leave. In addition to this, the Matron for the service will also be starting maternity leave in October. The Senior Leadership Team is working to recruit to all posts to ensure there is as little disruption as possible. We have seen a period of stability and improvement across the Red Kite View service and aim to sustain this despite the departure of key experienced and expert leaders. We wish them well and thanks for their service and leadership throughout our improvement journey.
2.3 – Assure
2.3.1 – Aspire provision of Early Intervention in Psychosis Services
The Head of Operations for our Community and Wellbeing Services continues to work with colleagues in Aspire to support improvements against the ‘treatment commencement’ targets. In August we are at 64% against a target of 60%.
Through the Service Development Improvement Plan (SDIP) the service has continued to maintain an improvement against the target for ‘referrals commencing packages of care within 2 weeks’, albeit with a slight decline in June (see Graph 12). With the SDIP and the changes made within the service, it is expected this improvement will be built on and maintained.
Graph 12

2.3.2 – Deaf CAMHS (Child and Adolescent Mental Health Services) Access to Assessment
As previously reported, waiting times and contacts have been the primary focus for Deaf CAMHS. The service’s leadership has completed a deep dive into the activity to determine what improvements can be made.
In recent years, Deaf CAMHS, in common with all Children & Young People’s Mental Health Services, has seen an increase in both demand and complexity. At the same time, there has been no uplift in funding. Effectively, the service is trying to deliver the same quality of service to significantly more children and young people than it was originally intended for. The original service specification (which is still current, though due for review) was designed for 104 referrals per annum. However, between January and April 2025, the caseload stood at over 200. The impact of this is that over the past 12 months, waiting times have increased.
The deep dive also identified that practice had not adapted at the same pace, and this is being addressed to ensure we maintain the quality of service provision whilst recognising a greater need for efficiency and productivity in the changing environment.
In addition, the service is conducting a full review of the caseload with a view to expediting discharge where appropriate. It is expected this will create capacity to increase contact and reduce waiting times. We have also identified areas of practice that have developed over time which are out of scope of the service specification (such as the service supporting families to work with Education, involving numerous meetings and often more than one member of staff at a time). Therefore, the service will look at directing these activities to more appropriate partners or will rationalise the level of involvement without compromising outcomes for young people.
Following the deep dive and initial interventions, there are already positive indicators of improvement. For example:
- The caseload in September has reduced to 171, a reduction of over 20% from April 2025
- The number of contacts has increased, June and July saw a two-year high of 167 and 179 contacts respectively. In contrast, the highest number of contacts in any one month for 2024 was 140. Over the year there has been a rate of increase in contacts of 20-25%. Deaf CAMHS activity contributes to one of the metrics for the NHS Oversight Framework (NOF), which currently has LYPFT in a positive position in Segment 2 (of 4), ranked 15 out of 61 non-acute Trusts.
In addition to addressing issues of practice and process, the Deaf CAMHS leadership is addressing workforce issues, including sickness absence rates, which has a disproportionate impact in a small highly specialised team. Sickness rates have steadily fallen from a high of 10.44% in March 2024 to 3.79% in July 2025.
The service is confident these improvements will be maintained and built upon. Two relatively new senior leaders in the service, the Deputy Director for Children and Young People’s Service and the Head of Operations, are now established and will monitor and support the service improvements.
2.3.3 – Rehabilitation Services
The formal consultation for the Complex Psychosis Pathway began on 1 August, with the expectation this will be concluded by 30 September. Several group sessions have been held, and there will also be individual meetings with line managers. Staff can feedback their views and ideas in relation to the proposed model and any impact on their role via these meetings and via email.
Consultation meetings have been supported by HR and Staffside. Feedback regarding the proposed model has been positive to date; however, some concerns have been expressed regarding changes from 5 to 7 day working, risks to Mental Health Officer status due to changes to job title, and increased demand on individual roles when working across teams. These are being fully reviewed and responded to. The consultation process has found historical gaps and variations in job descriptions which are being resolved and expected to be completed by 30 September.
3 – Service Developments
3.1 – Neighbourhood Developments
This section summarises the proposals for the development of a neighbourhood model within the NHS 10-year Health Plan (10YHP), drawing out the focus on mental illness; with an update on the Leeds application to be a pilot site through the National Neighbourhood Health Implementation Programme (NNHIP). Complimentary to the Neighbourhood Programme is the Neighbourhood Proactive Care Model Project and an existing project in relation to Mental Health and Long-term Conditions. There is also an update below for both of these.
3.1.1 – 10YHP Neighbourhood Model
The core element of the 10YHP is the Neighbourhood Health Services Strategy, moving care out of hospitals into local hubs. These hubs will bring together NHS teams, local government, social care and voluntary partners; embedding mental health into neighbourhood service models. The aim is to deliver earlier intervention; integrated, personalised care; improve access and reduce fragmentation; have fewer avoidable admissions and more holistic support. Success will depend on local leadership, sustained funding, and robust national support to guide implementation and measure outcomes.
These hubs will co-locate community psychiatrists, mental health nurses, therapists, peer support workers and other specialists alongside diagnostics, rehab and nursing services; to be open evenings and weekends. Outreach schemes staffed by community health workers and volunteers will proactively spot early signs of mental distress, reducing reliance on GPs and A&E and supporting prevention and early intervention locally.
Following a successful bid, Leeds has been named as one of the 43 local areas across the country in the first wave of the NNHIP, along with our West Yorkshire neighbours Wakefield and Bradford District and Craven. Partners from the Department of Health and Social Care, and NHS England will work with these 43 areas to accelerate learning and the implementation of neighbourhood health.
Key goals for participating in the programme are:
- To accelerate integrated, person-centred care (Communication, Coordination, Compassion)
- To develop new financial flows and contracting models
- To scale different neighbourhood hub models
- To influence national policy and address delivery barriers
- To develop expertise in linked data using the Leeds Data Model
- To develop innovation partnerships with the NHS, Council and universities
- To have strong public engagement and risk management experience
- To focus on the most deprived 20–26% of population to tackle health inequalities in alignment with Council priority neighbourhoods
- The development of VCSE, resident-led boards, and local funds to empower the local neighbourhoods.
Through the NNHIP, Leeds health and care partners will be working over the coming months to develop the programme further. Building on work already started in the city, in line with our Leeds ambitions and the Leeds Health and Wellbeing plan.
3.1.2 – The Neighbourhood Proactive Care Project
The Neighbourhood Proactive Care project aims to transform care delivery in Leeds by coordinating health and care provision to provide proactive, integrated, and person-centred care, closer to home. This should address issues of fragmentation, poor communication, duplication, and avoidable hospital or care home stays.
Using the Leeds Data Model to identify at risk populations, including those with mental illness, approaches will be tested across all providers collaborating at PCN and LCP level to deliver the following:
- Care coordination and case management
- Consistent care planning
- Out-of-hours support
- Falls prevention and proactive frailty management
- Integrated mental health and LTC support.
In the first year the key deliverables will be to:
- Establish networked multi-disciplinary teams
- Test care coordination “step up/step down” models
- Build strong cross-partner relationships in neighbourhoods
- Embed the continuous improvement approach.
It is expected this will deliver better health outcomes through prevention and maintaining independence, by reducing avoidable exacerbations. This should lead to better person, carer and staff experiences and ultimately to greater efficiency and system value. The LYPFT Older Peoples’ leadership team, the Physical Health Team and Community Mental Health Transformation Programme teams are embedded in this project. They will enable closer integration with community mental health services and Older Peoples’ services provided by LYPFT.
3.1.3 – The Neighbourhood Proactive Care Project
The Long-Term Conditions and Mental Health project (previously known as SEISMIC) is focused on the development of alternative integrated models of care to improve the health outcomes of people with three specific long-term conditions, one of which is Mental Illness.
The aim is to develop a flexible delivery model for proactive, patient-centred care across Primary Care Networks, underpinned by the Leeds Data Model, risk stratification, and integrated Multi-disciplinary Teams. The project has been successful in attracting health accelerator funding. This project focuses on getting people into, or to retain, or return to their employment by identifying those at risk, providing additional support through MDTs and joint care planning.
Burmantofts, Harehills & Richmond Hill Primary Care Network has been identified as a potential pilot site along with Seacroft. A workshop to design the delivery model is to be held towards the end of September. The project brings together the full range of health and care providers along with academics from the Leeds universities and the ICB to ensure there is a robust research framework around this programme. This is expected to build a body of clinically-based evidence in this field.
3.2 – Third Sector Contracts.
The Trust holds 21 sub-contracts with other providers with an annual contract value of approximately £6 million. With the introduction of the new Health Care Services Provider Selection Regime Regulations (PSR 2023), we are reviewing these contracts and have developed a governance process to ensure compliance with the new guidance.
The three processes that can be used to award a contract under the PSR 2023, are:
- Direct Award
- Most Suitable Provider Process
- Competitive Process.
The services range in nature including our Early Intervention in Psychosis contract, the Accommodation Gateway and Memory Support Worker Contracts, and Harm Reduction Workers as well as a range of other services.
The review process is underway and will be concluded within quarter 3 of 2025/26.
3.3 – Draft Planning Guidance
NHS England has published a draft planning guidance framework. The framework introduces a structured, multi-year, integrated planning approach for the NHS. The framework aims to ensure financial sustainability, stronger collaboration across organisations, and alignment with the 10-Year Health Plan priorities which are: shifting care to the community; leveraging technology; and improving population health. It shifts planning from annual cycles to a rolling five-year horizon enabling long-term, integrated financially sustainable planning.
The guidance is based on a number of key principles:
- Outcome-focused: deliver measurable improvements for patients, public, and taxpayers
- Accountable and transparent: clear roles, responsibilities, and governance
- Evidence-based: plans grounded in data, modelling, and best practice
- Multi-disciplinary: finance, workforce, clinical, and other functions involved
- Credible and deliverable: ambitious but realistic, with risks and constraints addressed.
NHS England and the Department for Health and Social Care will set the priorities, frameworks and guidance, with regions coordinating cross-system planning and assuring plans. ICBs will be the strategic commissioners overseeing population health, inequalities, access and resource allocation.
ICBs will also produce five-year strategic commissioning plans, with providers producing five-year integrated delivery plans. Local Authorities will be required to produce neighbourhood health plans, that will be local authority led, integrating NHS, Social care, VCSE and public health.
Care services will work with the Programme Management Office, the Finance Team and clinical services to commence the implementation and updates will be provided as the work progresses.
4 – Emergency Prepardeness Resilience and Response
4.1 – Incidents and Disruptions
4.1.1 – Heatwave Response
The Trust responded well to the heat health alerts on 10-15 July and 11-18 August. Tactical level planning arrangements had been in place since May, to monitor and manage periods of heatwave. Measures to mitigate the risks were put in place and staff awareness was raised via the Communications Team. Since June no further additional spend has been needed to purchase portable air conditioning units to mitigate the risk in the summer period.
4.1.2 – NRS Healthcare
NRS Healthcare (also known as Nottingham Rehab Ltd) went into liquidation on 1 August 2025. This company provided equipment to NHS providers and Local Authorities across the country. Most recent figures produced by the Procurement Team identified a relatively modest spend specific to LYPFT and equates to around 150 orders of equipment over the year. Intelligence suggests that impacts are being felt more keenly by providers in the south of England.
A tactical group has been formed to gather information for the Trust, assess any risks and identify options and contingencies. This group includes representatives from all services and the Procurement Team.
NRS provided the Trust with OT equipment for use in the community and inpatient settings. Areas of potential risk are around the ordering of new equipment for use on Trust premises such as inpatient wards, repair and maintenance of such equipment and also the provision, maintenance and repair of equipment used by service users in their own homes.
Some services are currently using a range of alternative suppliers. This can be time consuming since these suppliers may not have supplied the NHS in the past. In order to minimise risks, services are seeking specialist advice and exercising professional judgement to ensure that equipment is safe and appropriate.
The Trust’s Procurement Team is to provide our services with guidance, listing alternative suppliers and where they may be used. They have also identified a person who will act as a single point of contact for services to aid consistency of response.
Services have been asked to gather intelligence and report back to the tactical group on a fortnightly basis about any issues they are experiencing around maintenance and repair of equipment, both in Trust premises and that used by service users in the community. This will inform advice that will be given to our service users.
4.1.3 – Industrial Action
The Trust planned for and responded to industrial action by members of the BMA between 07:00 on Friday 25 July and 07:00 on Wednesday 30 July. All rotas were covered by Resident Doctors and there was no requirement to ask for senior doctors to cover. A small number of memory assessment clinics in the Older Peoples’ Service were cancelled, with appointments re-arranged as soon as possible thereafter.
Although the BMA agreed there would be no strikes in August, they hold a mandate for industrial action by Resident Doctors which lasts until January 2026.
An indicative ballot undertaken by SAS (Specialty, Associate Specialist, and Specialist doctors) and Consultant BMA members has also been completed. The ballots, which were conducted between 21 July and 1 September, revealed that 67 per cent of consultants and 82 per cent of SAS doctors were willing to strike. This was based on a turnout of approximately 50%. No plans for a formal ballot have yet been announced.
RCN members voted in an indicative ballot to reject a 3.6% pay increase proposed by the government. The RCN has yet to trigger a formal ballot for strike action.
The Trust continues to monitor the situation and is holding fortnightly strategic coordinating meetings to oversee tactical response to industrial action. If industrial action is announced, then response arrangements will be established following models used in July and previous periods.
4.1.3 – Demonstrations
The EPRR Team continues to monitor the situation with regard to demonstrations that have been taking place in several parts of the Leeds district over the past 5 weeks. Staff have been made aware of where such demonstrations will take place, so they are able to take safety precautions if they are visiting the area. Communications have also been issued to staff to ensure they are aware of any disruption caused by planned demonstrations in central Leeds.
4.1.5 – Exercise Pegasus
In September, October and November the Trust will be participating in a national pandemic response exercise, known as Exercise Pegasus. The Chief Operating Officer and the Director of Nursing will be taking part in the exercise along with the EPRR team. Lessons identified in the exercise will be used to improve planning and response to a future pandemic.
5 – Summary and Recommendation
We continue to manage and lead a response to a range of challenges in the delivery of consistent and sustainable high-quality care for all people needing our support through a whole system approach. The report highlights the most significant service delivery and development challenges we face but importantly sets out where service delivery has stabilised or where improvements have been made in Care Services.
The Board is asked to be assured of the work being undertaken to deliver our Care Services and to manage the range of challenges and issues outlined in this report.
Joanna Forster Adams
Chief Operating Officer
September 2025
Contributions from members of the Care Services’ Senior Operational Leadership Team.
Service Performance Report June 2025
Please download the Service Performance Report August 2025. This PDF is not accessible to some users, please see below plain text summaries of the document.
Access and Responsiveness: Our Response in a Crisis
-
- ALPS referrals within 1 hour: Slight improvement in August (64.2%) from July (60.2%), but below June (72.5%).
- S136 detentions over 24 hours: Consistently 0 across all months.
- Crisis referrals seen within 4 hours: Declining trend from June (69.7%) to August (58.3%), below the 90% target.
- CRISS caseload under 6 weeks: Strong performance, consistently above target (86.7% in August).
- CRISS users seen 5+ times in first week: Below target, steady around 33%.
- CRISS referrals from acute inpatients: Fluctuating, 8.7% in August.
Access and Responsiveness to Learning Disabilities, Regional and Specialist Services
- Gender Identity Service waiting list: Increased to 6,899 in August.
- Deaf CAMHS wait time: Rose to 225.55 days in August.
- Community LD referrals seen within 4 weeks: Improved to 69.7%, close to 75% target.
- LADS diagnostic decision within 26 weeks: 64.7% in Q1.
- LADS assessment within 13 weeks: Low at 14.5% in Q1.
- CAMHS inpatient assessments within 7 days: 81.2% in Q1, below 100% target.
- Perinatal urgent contact within 48 hours: 75% in Q1.
- Perinatal routine referrals within 2 weeks: 87.5% in Q1, above target.
- Distinct women seen (rolling 12 months): 936 in Q1, close to target of 950.
- Perinatal DNA rate: 8.5% in Q1.
Our Acute Patient Journey
- Under-16 admissions to adult facilities: 0 across all months.
- CAU bed occupancy: High, 84.9% in August.
- CAU length of stay: Decreased to 11.17 days in August.
- Liaison In-Reach assessments within 24 hours: 84.9% in August, below 90% target.
- Adult acute bed occupancy: Consistently over 100%.
- Ward-specific occupancy: All wards above 99%, some exceeding 105%.
- Older adult occupancy: Increased to 91.3% in August.
- Clinically ready for discharge: Dropped to 29.6% in August.
- Out of area placements: 36 active placements in August, above trajectory of 11.
- Out of area bed days: Increased to 1,037 in August.
Our Community Care
- Follow-up within 3 days (Trust-wide): 85.0% in August, above target.
- Follow-up within 3 days (HCP only): 84.7% in August.
- Community mental health caseload: 3,522 in August.
- Memory service referrals seen within 8 weeks: 80.9% in Q2, above target.
- Memory service diagnosis within 12 weeks: 50.4% in Q2, just above target.
- EIP/ARMS treatment within 2 weeks: 64.3% in August, above target.
- EIP discharge to primary care: 67.2% in Q1.
- EIP cardiometabolic assessments: 54.3% in Q1, below 80% target.
Clinical Record Keeping
- NHS number recorded: 99.7% consistently.
- Ethnicity recorded: 81.1% in August.
- Sexual orientation recorded: 45.5% in August.
- DQMI (MHSDS quality): 90.6% in April, below 95% target. No data for May due to submission issue.
Cover sheet for Winter Plan Board Assurance Statement
- Paper title: Winter Plan Board Assurance Statement
- Date of meeting: 25 September 2025
- Presented by: Joanna Forster Adams, Chief Operating Officer
- Prepared by: Mark Dodd, Deputy Director of Operations
This paper supports the Trust’s strategic objective/s (SO):
- SO1 – We deliver great care that is high quality and improves lives.
- SO2 – We provide a rewarding and supportive place to work.
- SO3 – We use our resources to deliver effective and sustainable services.
This paper relates to the Trust’s strategic risks (SR):
- SR7 – Plan and deliver services that meet the health needs of the population we serve.
Executive summary
The purpose of the Winter Resilience and Operating Plan is to set out the approach the Trust will take to maintaining service provision and minimising disruption during the winter of 2025/26.
This year, in addition to the production and submission of the Plan, there is a requirement from NHS England that the Trust provides a Board Assurance Statement to ensure the Board has had oversight of the Plan and that all considerations have been met in its development. The Board Assurance Statement and related documentation have been attached to facilitate the Board’s considerations.
Once the Board is assured the content of the Plan meets the requirements, it needs to agree the Board Assurance Statement can be signed (on its behalf) by the Chair and Chief Executive (see signature block at the bottom of page 4 of Appendix 1) prior to the Plan and Statement being submitted to the UEC Team at NHS England before the 30 September 2025 deadline.
Do the recommendations in this paper have any impact upon the requirements of the protected groups identified by the Equality Act? No
Recommendation
The Board is asked to:
- Receive and review the Winter Plan Board Assurance Statement and associated documentation
- Be assured that the content of the Plan meets the requirements as set out in the Statement
- Agree that the Board Assurance Statement can be signed on its behalf via the electronic signature of the Chair and Chief Executive, prior to submission to the UEC Team at NHS England before 30 September 2025 deadline.
Winter Plan Board Assurance Statement
1 – Executive summary
The purpose of the Winter Resilience and Operating Plan is to set out the approach the Trust will take to maintaining service provision and minimising disruption during the winter of 2025/26.
This year, in addition to the production and submission of the Plan, there is a requirement from NHS England that the Trust provides a Board Assurance Statement to ensure the Board has had oversight of the Plan and that all considerations have been met in its development. The Board Assurance Statement and related documentation have been attached to facilitate the Board’s considerations.
- Once the Board is assured the content of the Plan meets the requirements, it is asked to agree that the Board Assurance Statement can be signed on its behalf via the electronic signature of the Chair and Chief Executive, prior to submission to the UEC Team at NHS England before 30 September 2025 deadline.
2 – Introduction
During winter 2025/26, Systems will be expected to maximise opportunities to continue to support the NHS recovery programme whilst also ensuring continued application of the UK Infection Prevention and Control guidance to prevent and control infection, and to respond to additional demands and pressures as they arise.
It is recognised that Winter Plans will need to be integrated and developed in partnership across each System, but also iteratively and be able to adapt to competing demands as we move through the winter period.
Now, more than ever we know that effective resilience will only be achieved during the winter period through effective system and partnership-working with our NHS, social care, third sector, VCSE partners, with the public, with the people that use our services, and with our staff.
The Plan details the Trust’s Operating Objectives for the winter period, the arrangements in place to effectively manage clinical and operational delivery of services, and the actions that will be taken to mitigate anticipated risks during this period.
3 – Board Assurance Statement (BAS)
This year there is a requirement from NHS England that the Trust provides a Board Assurance Statement to demonstrate the Board has oversight of the Winter Plan and all considerations have been met in its development.
The BAS describes the approach to creating the Plan and demonstrates how links with other aspects of planning have been considered. The Board Assurance Statement is attached at Appendix 1 (Section A) for the Board’s consideration.
This Statement is accompanied by a checklist referencing where in the Plan each of the requirements set out below has been included. These elements cover:
- Capacity: There is evidence of modelling of demand and responding to the demand surges with robust plans to manage capacity and flow. There are also sufficient staff available at times of expected increase in demand
- Responsiveness: Ensuring urgent mental health services are operationally resilient to be able to respond to increased demand. All service users who are considered high risk, or are frequent users of urgent care services, have robust crisis plans in place ahead of winter.
- Leadership: Robust on-call arrangements are in place to always support responses to real time pressures, including the use of the OPEL framework.
- Prevention: There is a plan in place to improve at least a 5% increase in the uptake of the flu vaccination by frontline staff
- Infection Prevention and Control: IPC colleagues have contributed to the plan and have developed plans for delivering ‘Fit Testing’ for frontline staff, ensuring PPE stock is available as required and have appropriate escalation plans in place for any potential outbreaks
The checklist is part of Appendix 1 (section B).
4 – Our process for development
In developing our Plan, we have engaged with key strategic and operational leads to ensure the content reflects what we need in place to meet the challenges of winter.
Internally we have engaged with a number of key leads including the EPRR Lead, the Associate Director for Employment, the Head of Health Equity, the Patient Experience Team with links to the SUN Network, and the Communications Team. Any comments received have been considered and used to inform the Plan.
We have also presented the Plan to members of the Strategic Co-ordination Group for their consideration and comment.
The Plan is Appendix 2.
5 – Conclusion
The Board is asked to be assured that the Winter Resilience and Operating Plan for 2025/26 meets the requirements as set out in the Board Assurance Statement and the related checklist, and that it has been through a robust governance process to ensure it describes how our services will operate effectively during the winter period and meet the needs of our service users.
6 – Recommendation
The Board is asked to:
- Receive and review the Winter Plan Board Assurance Statement and associated documentation
- Be assured that the content of the Plan meets the requirements as set out in the Statement
- Agree that the Board Assurance Statement can be signed on its behalf via the electronic signature of the Chair and Chief Executive, prior to submission to the UEC Team at NHS England before 30 September 2025 deadline.
Mark Dodd
Deputy Director of Operations
September 2025
Appendix 1 Winter Planning 25/26 – Board Assurance Statement (BAS) NHS Trust
Section A: Board Assurance Statement
Governance
| Assurance statement | Confirmed (Yes / No) | Additional comments or qualifications (optional) |
| The Board has assured the Trust Winter Plan for 2025/26. | Yes | The Winter Plan for 2025/26 has been through a comprehensive process of governance for its development and approval, which has involved all key operational and strategic leads, and is presented to the September 2025 Board meeting for final sign off. |
| A robust quality and equality impact assessment (QEIA) informed development of the Trust’s plan and has been reviewed by the Board. | Yes | The initial EHIA screening has been used and indicates that a full EHIA is not required, see Appendix A in the Winter Plan. |
| The Trust’s plan was developed with appropriate input from and engagement with all system partners. | Yes | The plan has been developed in conjunction with ICB led arrangements for winter planning and with system partners, including LTHT, LCH, LCC, GP Confed and VCSE. |
| The Board has tested the plan during a regionally-led winter exercise, reviewed the outcome, and incorporated lessons learned. | Yes | The plan has been developed through the ICB engagement events, and we have contributed to the ICB plan that has been tested at a NHSE regional held event on the 3 September 2025. Whilst NHSE had further questions about the regional plan, these were centred on the Acute Trust elements with no further actions for LYPFT and their plan. |
| The Board has identified an Executive accountable for the winter period, and ensured mechanisms are in place to keep the Board informed on the response to pressures. | Yes | Joanna Forster Adams, Chief Operating Officer, is the Accountable Emergency Officer responsible for delivering the Winter Plan and reporting to Board. The Board will be kept informed through either the COO report or exception reporting (where this is necessary) and matters for advice or escalation to the Board will be identified through the comprehensive operational governance structure and procedures in place. |
Plan content and delivery
| Assurance statement | Confirmed (Yes / No) | Additional comments or qualifications (optional) |
| The Board is assured that the Trust’s plan addresses the key actions outlined in Section B. | Yes | Please see the Winter Plan Checklist (part of this document below) which demonstrates how these requirements have been met. |
| The Board has considered key risks to quality and is assured that appropriate mitigations are in place for base, moderate, and extreme escalations of winter pressures. | Yes | The risks are detailed in the plan with mitigations recorded and plans for monitoring and escalation are in place. See section 2.6.2 and 3.4 of the Winter Plan. |
| The Board has reviewed its 4 and 12 hour, and RTT, trajectories, and is assured the Winter Plan will mitigate any risks to ensure delivery against the trajectories already signed off and returned to NHS England in April 2025. | Yes | We will maintain service delivery throughout winter as normal unless demand in our priority services requires the need to deploy resources to support them. See section 3.2. |
Section B: 25/26 Winter Plan checklist
Prevention
| Checklist | Confirmed (Yes / No) | Additional comments or qualifications (optional) |
| 1. There is a plan in place to achieve at least a 5 percentage point improvement on last year’s flu vaccination rate for frontline staff by the start of flu season. | Yes | Please see section 5.2 of the Plan. |
Capacity
| Assurance statement | Confirmed (Yes / No) | Additional comments or qualifications (optional) |
| 1. The profile of likely winter-related patient demand is modelled and understood, and plans are in place to respond to base, moderate, and extreme surges in demand. | Yes | Please see section 2 of the Plan. |
| 2. Rotas have been reviewed to ensure there is maximum decision-making capacity at times of peak pressure, including weekends. | Yes | Please see section 4 of the Plan. |
| 3. Seven-day discharge profiles have been reviewed, and, where relevant, standards set and agreed with local authorities for the number of P0, P1, P2 and P3 discharges. | Yes | We do plan across 7 days for discharge and have recently introduced 7-day bed management. However, as discharges are medically led and our inpatient Consultants and SAS doctors do not work across 7 days, discharge rates are slower over weekends. This is part of our ongoing IPF improvement programme. We can also confirm that the P0, P1, P2 and P3 discharges do not apply to mental health services at this time but is an area of work being developed with system partners. |
| 4. Elective and cancer delivery plans create sufficient headroom in Quarters 2 and 3 to mitigate the impacts of likely winter demand – including on diagnostic services. | Not applicable | N/A |
Infection Prevention and Control (IPC)
| Assurance statement | Confirmed (Yes / No) | Additional comments or qualifications (optional) |
| 1. IPC colleagues have been engaged in the development of the plan and are confident in the planned actions. | Yes | Please see section 5 of the Plan. |
| 2. Fit testing has taken place for all relevant staff groups with the outcome recorded on ESR, and all relevant PPE stock and flow is in place for periods of high demand. | Yes | Please see section 5.3 of the Plan. |
| 3. A patient cohorting plan including risk-based escalation is in place and understood by site management teams, ready to be activated as needed. | Yes | Please see section 5.4 of the Plan, as per outbreak procedures. |
Leadership
| Assurance statement | Confirmed (Yes / No) | Additional comments or qualifications (optional) |
| 1. On-call arrangements are in place, including medical and nurse leaders, and have been tested. | Yes | Please see sections 3.1, 4.1 and 7.2 of the Plan. |
| 2. Plans are in place to monitor and report real-time pressures utilising the OPEL framework. | Yes | Please see sections 2.6, 3.4, and 4.1 of the Plan. |
Specific actions for Mental Health Trusts
| Assurance statement | Confirmed (Yes / No) | Additional comments or qualifications (optional) |
| 1. A plan is in place to ensure operational resilience of all-age urgent mental health helplines accessible via 111, local crisis alternatives, crisis and home treatment teams, and liaison psychiatry services, including senior decision-makers. | Yes | Please see sections 2 and 3 of the Plan. |
| 2. Any patients who frequently access urgent care services and all high-risk patients have a tailored crisis and relapse plan in place ahead of winter. | Yes | Please see section 2.3 of the Plan. |
Winter Resilience and Operating Plan 2025/26
Contents
Introdcution
Maintaining flow and meeting demand
- 2. Maintaining flow and meeting demand
- 2.1 Acute capacity and flow
- 2.2 WAA out of area trajectory
- 2.3 ED waits for MH assessment
- 2.4 Crisis Resolution and Intensive Support Service (CRISS)
- 2.5 Community Services
- 2.6 Responding to surge and demand
- 2.6.1 Service prioritisation
- 2.6.2 Key risks and mitigations
Winter management arrangements
- 3. Winter management arrangements
- 3.1 Current service provision and prioritisation
- 3.2 Activity and performance management
- 3.3 Service line assurance report
- 3.4 System level winter arrangements
Winter staffing
Supporting the health of our people and patients over the winter
- 5. Supporting the health of our people and patients over the winter
- 5.1 Previous seasonal vaccination campaign
- 5.2 Autumn/winter 2025-26 vaccination plan
- 5.2.1 Publicising the campaign
- 5.3 Fit Testing
- 5.4 Outbreak management
Addressing health inequalities
EPRR response
- 7. EPRR response
- 7.1 Winter coordination
- 7.1.1 Strategic Coordination Group
- 7.1.2 Tactical Coordination Group
- 7.2 Adverse weather
- 7.3 Other winter risks
- 7.3.1 Power disruption
- 7.3.2 Maintaining access to Trust sites
- 7.3.3 Equipment shortages
Conclusion
- 8. Conclusion
- Glossary
- Appendix A: Initial EHIA Screening
- Appendix B: Service Priority Categorisation
- Appendix C: Service Line Assurance Report
- Appendix D: Staffing escalation and deployment protocol
- Appendix E: Mental Health ED Flow Action Cards
1. Introduction
The purpose of the Winter Resilience and Operating Plan is to set out the approach that Leeds and York Partnership NHS Foundation Trust (the Trust) will take to maintaining service provision and minimising disruption during the winter of 2025/26.
During winter 2025/26, Systems will be expected to maximise opportunities to continue to support the NHS recovery programme whilst also ensuring continued application of the UK Infection Prevention and Control guidance to prevent and control infection, and to respond to additional demands and pressures as they arise.
It is recognised that Winter Plans will need to be integrated and developed in partnership across each System, but also iteratively and be able to adapt to competing demands. Now, more than ever we know that effective resilience will only be achieved during the winter period through effective system and partnership-working with our NHS, Social Care, Third Sector / VCSE partners, with the public, with the people that use our services, and with our staff.
An Equality and Health Inequalities Impact Assessment (EHIA) was undertaken when developing this plan to determine its impact on people at risk of health inequalities, see appendix A. The initial screening indicates that a more detailed assessment was not required.
The Plan details the Trust’s Operating Objectives for the winter period, the arrangements in place to effectively manage clinical and operational delivery of services, and the actions that will be taken to mitigate anticipated risks during this period. This includes:
- Operating Principles
- Maintaining capacity and flow
- Responding to surge and demand
- The identification of risks to critical services
- Maintaining the wellbeing of our staff and service users
- Links to EPRR structure and wider system incident response.
1.1 Operating principles
In line with national guidance and developed System plans, we have several operating principles and objectives that underpin our Winter Plan, building on learning from previous years. Our operating principles and aims are to:
- Minimise disruption to service users, carers and our staff
- Maintain access, responsiveness, and flow through services, in partnership where this is required, ensuring emergency access / urgent care is sustained throughout
- Maintain and protect safe, high quality service delivery
- Maintain all elements of service delivery in accordance with our agreed and current operating models wherever possible
- Continue to deliver all services for as long as is practicable in times of increased escalation, and any suspended or restrictions to services being recovered as soon as is possible
- Continue to develop and implement sustainable and effective services that can respond to ‘on the day’ demands of the population
- Seek to actively identify and address health inequalities across our services and the specific challenges faced by minority groups
- Ensure proactive leadership and management arrangements are in place that allow us to continue to adapt and respond as things change
- Use robust on-call arrangements to provide leadership and management outside of normal working hours
- Support our staff to prepare for and respond to the pressures and challenges we face through winter, actively promote and support staff’s physical and mental wellbeing to ensure enhanced and ongoing resilience, including access to Flu vaccinations
- Work as a proactive system partner, ensuring clear integrated plans and governance structures are in place for early escalation and mitigation of emerging / unexpected / external pressures
- Ensure that our contingency plans and emergency measures are evaluated to understand the impact they will have and mitigate risks wherever possible.
2. Maintaining flow and meeting demand
2.1 Acute capacity and flow
Our acute mental health service has continued to face considerable challenges throughout the year, including sustained high demand, constrained bed capacity, and increasingly complex discharge pathways. In response, we are driving forward the Inpatient Quality Transformation Programme, which is structured around three key workstreams: Improving Flow, Culture of Care, and a comprehensive Review of Acute Care Pathways.
Key priorities within the Improving Flow workstream include:
- Reducing Length of Stay – Implementing evidence-based interventions to safely reduce the average length of inpatient admissions, including enhanced discharge planning from the point of admission and daily multidisciplinary reviews.
- Strengthening Admission and Discharge Processes – This includes the use of new roles to support discharge including discharge coordinators and Housing Officers.
- Delivering a 7-day bed management function – This enables proactive management of capacity and flow.
- Reducing Out-of-Area Placements – Working with system partners to expand capacity in community-based alternatives, reducing reliance on external providers and maintaining continuity of care.
Our comprehensive Review of Acute Care Pathways includes a full evaluation of how individuals’ access, experience, and transition through acute mental health services. This review is designed to ensure that pathways are clinically effective, person-centred, and aligned with both national models and local system priorities.
We envisage this work will begin to show measurable impact by winter, as redesigned pathways, improved flow mechanisms, and cultural enhancements become embedded across our acute mental health services. By aligning improvements with compassionate, values-driven care, we aim to create a more responsive and resilient system that better meets the needs of service users, carers, and staff. The changes introduced through the Inpatient Quality Transformation Programme will support safer admissions, more timely discharges, and a more therapeutic inpatient experience laying the foundation for sustained improvement across future winter periods.
Last winter we saw a reduction in female admissions compared to previous years, and yet an increase for the male population over the same period (see Graphs 1 and 2). There is no indication there are seasonal trends that can be attributed to this or planned for.
Graph 1
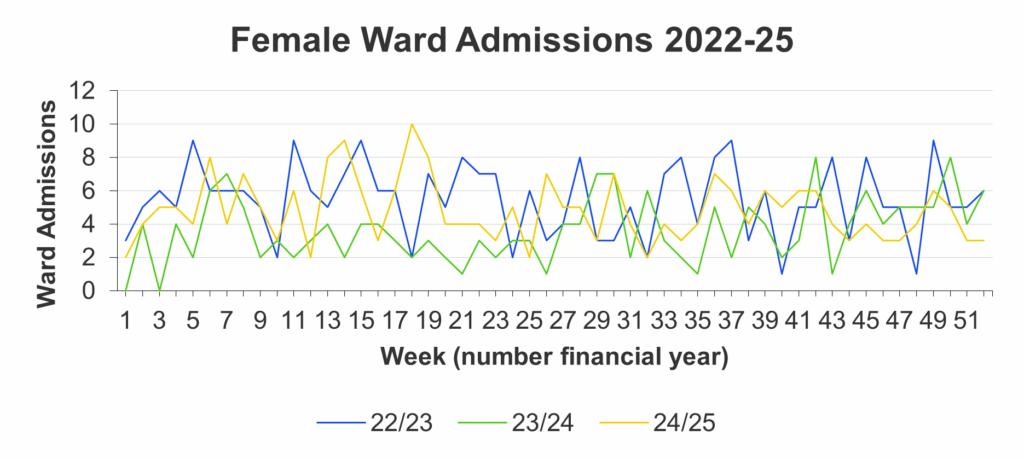
Graph 2
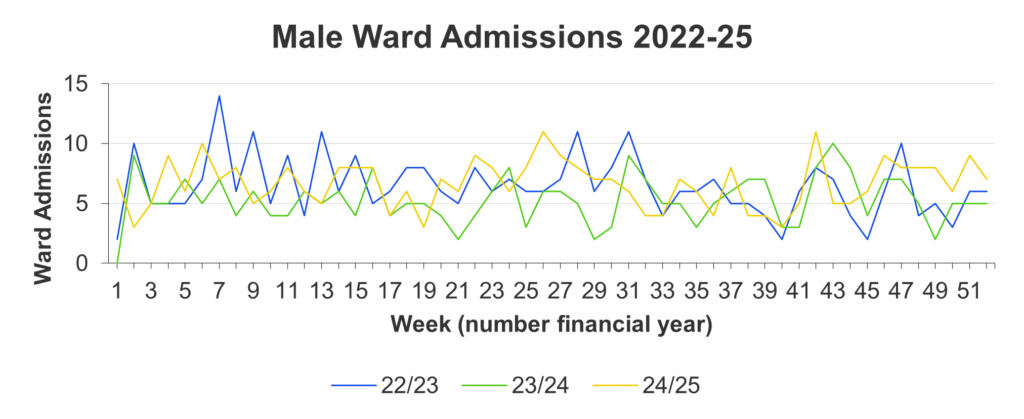
2.2 WAA out of area trajectory
During 2024/25 the Inpatient Flow Programme made significant progress in reducing the number of Out of Area (OOA) placements, compared to the previous year, and we were generally able to meet the trajectory that was set. However, as we were coming out of winter last year, we saw a surge in demand for inpatient admissions resulting in an increase in OOA placements (see Graph 3). This pressure is largely driven by consistent demand for admissions, alongside delays in discharging patients who are clinically ready. A key contributing factor to these delays is the limited availability of appropriate accommodation, particularly supported housing, which prolongs inpatient stays and reduces the availability of beds for new admissions. This is an issue that has been highlighted at a Leeds system level, and any actions will form part of the winter planning for 2025/26.
Graph 3
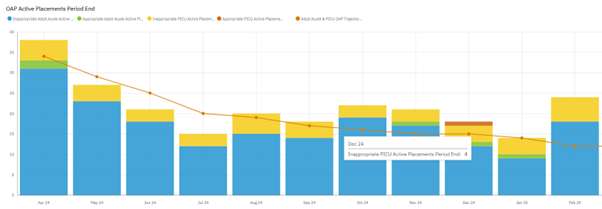
As we can see from Graph 4, we are unable to achieve our planned trajectory to reduce OOA placements through 2025/26, which as we approach winter will increase pressure and reduce our ability to maintain our capacity and flow. The Inpatient Quality Transformation Programme Oversight Group has a clear focus on reducing the number of OOA placements with a number of actions to achieve this.
Graph 4
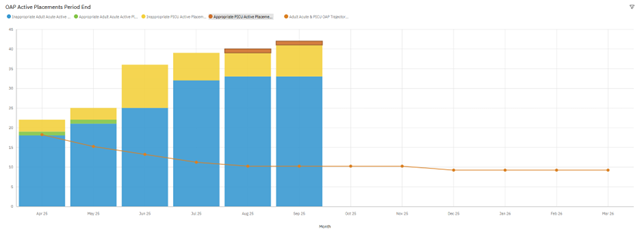
Weekly Clinically Ready for Discharge (CRfD) meetings are chaired by the Head of Operations for the Working Age Adult (WAA) Acute Service, which will be responsible for any escalations required within the Trust and the wider Leeds system. The meetings will also have representation from Adult Social Care, Housing and the Leeds office of the ICB. The service is exploring the role of hospital based Social Workers with Adult Social Care to facilitate discharges for those service users with social care needs.
To support discharges, Mini-MaDE meetings are now embedded, with encouraging levels of engagement from community services and system partners. This collaborative approach is fostering improved communication and shared decision-making, which is expected to support timelier and coordinated discharge planning. This approach will continue throughout the winter period with the ability to escalate any pressures that may occur because of increased winter pressures within the wider system.
The WAA Adult Acute Service continues to work with the ICB on the three previously identified areas where support is required:
- System visibility / operational oversight to support discharge management
- Access to housing and supported accommodation
- Access to third sector support.
2.3 Emergency Department (ED) waits for mental health assessment
Throughout the winter of 2024/25 we continued to face challenges in the ability to transfer service users to mental health beds, which resulted in some long delays for admissions including those in the Emergency Department (ED) within LTHT. The need to reduce the length of waiting time for people who require admission to mental health inpatient treatment, is a priority area of work and is an imperative as part of the planning requirements for winter 2025/26. The programme to address this is broadly divided into three key areas:
- Reducing Mental Health ED Attendances and Delays Project Oversight Group: This group has been formed to collaborate across care services, enhancing systems, processes, and communication. It will consist of several workstreams focused on data analysis, NHS England ED action cards, communication, and internal processes. Initial work includes a process mapping exercise to thoroughly understand current escalation procedures and identify opportunities for efficiency.
- Regular improvement meetings with Leeds Teaching Hospitals Trust (LTHT) Colleagues: We have initiated regular meetings with colleagues from LTHT to address challenges in meeting demand and maintaining flow through Emergency Departments. This group includes Business Intelligence colleagues who are working to develop a shared data set to ensure consistency and provide reliable oversight of activity. The group is developing a shared escalation and action plan to minimise delays and improve communication.
- Leadership of Acute Liaison Psychiatry Service (ALPS): The leadership team for the ALPS has focused on improving their response times, achieving some progress while recognising the need for further improvements.
On average ALPS has seen an increase in the rate of activity each year, but it does not follow a clear seasonal pattern (see Graph 5). Data for the year 2024/25 showed a reduction in referrals over the winter period, with higher demand in summer (see Graph 6).
We also saw an increase in the time from arrival to the ED and the referral to ALPS during the winter months (see Graph 7). We know that overall, ED attendances have increased over this period, and we can assume that the delays in referrals to the ALPS team are because of this increased activity and subsequent delays in triaging service users. The ALPS team are exploring how this might be improved on, including the potential use of a mental health triage system.
We will ensure that service users who have been identified as those who frequently use urgent care services and are considered high risk, have robust crisis / relapse plans in place to ensure we are responsive to their needs ahead of winter to reduce the demand on our ED services.
We did see an increased delay in the response time for assessment by the team over the past winter (see Graph 8), which is partly a result of vacancies and sickness absence. The team is in the process of recruiting to vacant posts and is expected to be fully staff ahead of this next winter.
Graph 5
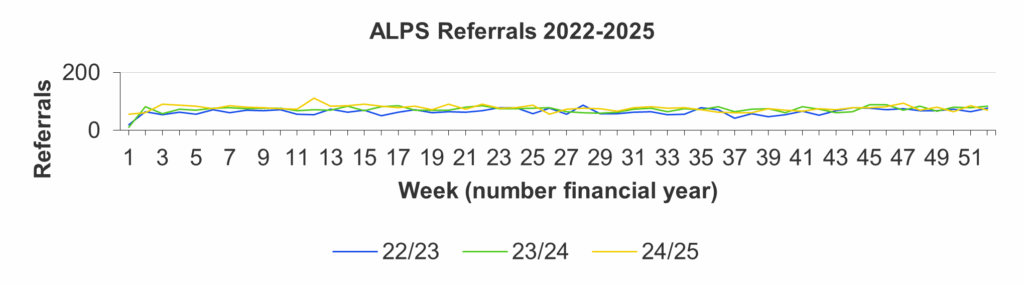
Graph 6

Graph 7
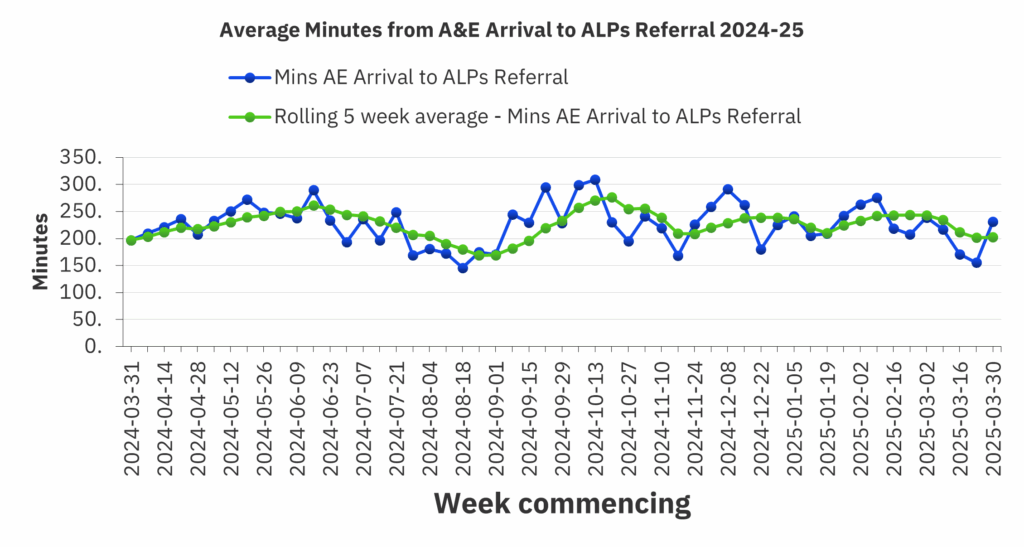
Graph 8

2.4 Crisis Resolution and Intensive Support Service (CRISS)
CRISS provides a rapid response to service users who are experiencing an acute crisis in the community and is an alternative to hospital admission. This service is vital to reduce the demand for the inpatient service, to maintain capacity for those who require an inpatient stay at the point of need.
The CRISS service has different response times based on the priority of the response required, 4 hours and 24 hours. The service has struggled to meet the Key Performance Indicators (KPI) of 90% compliance against the targets throughout the past year since the service change due to staffing issues including sickness and vacancies (see Graphs 9 and 10). There is a plan in place to support improvement against the KPIs, and we anticipate a significant improvement as we head towards winter. Team Managers are reporting to the Senior Leadership team on a weekly basis to monitor progress and identify actions that can be taken to improve response times, which includes moving the resource across the three areas. The service is actively recruiting staff to vacancies, and we expect all posts to be filled by the start of winter.
Graph 9 – Referrals seen for MH assessment within 4hrs

Graph 10 – Referrals seen for urgent assessment within 24hrs

We have seen a consistent rate of referrals to this service over the past 3 years with a slight decrease early in the winter of 2024 (see Graph 11). We anticipate this to continue through to mid-2026/27. However, we have seen a return to the number of contacts for those service users under the care of CRISS to early 2022 levels following a reduction in late 2022/23 and mid-2023/24. We anticipate the number of contacts increasing over this next winter to mid-2026/27.
Graph 11

The service will continue to monitor levels of activity to ensure it is able to make improvements against its performance targets so we are responsive and alleviate any pressure that may result in other parts of the system.
2.5 Community Services
We will also ensure that our community-based services maintain the level of service that meets the needs of those we care for throughout the winter period, particularly over the holiday season. We do not expect any service to close during this period, and by taking this approach, we do not expect an increase in attendances to the ED or an increase in referrals to our crisis services because of service users being unable to access their usual support networks.
Whilst we have seen an increase in referrals to our Adult Community Mental Health Teams over the past year compared to previous years (see Graph 12), we expect to see a reduction in referrals in the early weeks of winter with a steady return to normal levels as winter ends.
Graph 12
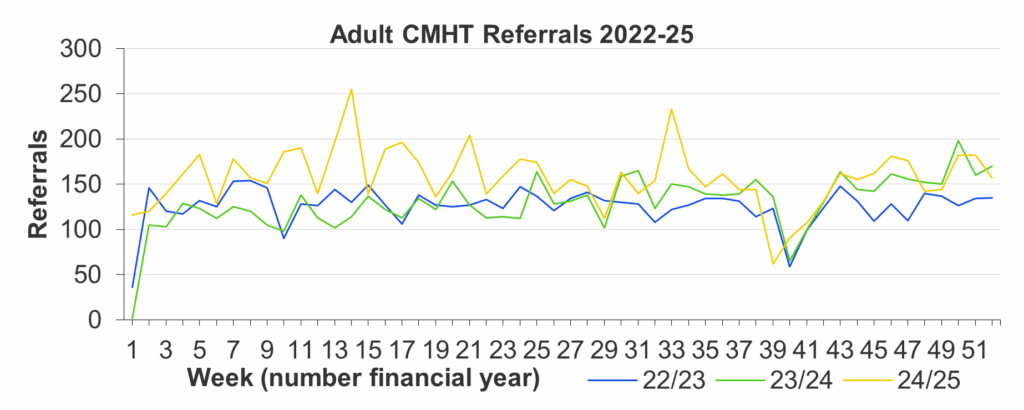
2.6 Responding to surge and demand
The analysis of data relating to activity throughout the year for the past three years shows that we do not generally experience surges in demand as a result of winter. We do though, experience increased demand and surges at various points throughout the year, but these are not identifiable as seasonal trends and have not been significant enough to require additional resources being allocated in these areas.
Should any increased surge and demand warrant additional resources being mobilised to support a particular area, we will use the service prioritisation system to identify the suitable resources to deploy. This will be coordinated and managed through the Trust’s Strategic Coordination Group (SCG) which will be stood up ahead of winter to manage all winter pressures. These real time pressures are monitored through the Trust’s Operational Dashboard (see example at Diagram 1) and the Operational Pressures Escalation Levels (OPEL) framework. We will also use the Mental Health Action Cards to support decision making, (see Appendix E).
Diagram 1
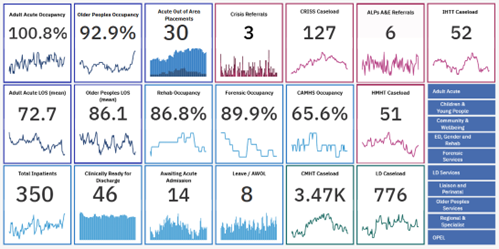
2.6.1 Service Prioritisation
We have an established and agreed process of service prioritisation as part of our EPRR business continuity approach. This identifies which services are an essential priority and required to always be maintained at full capacity and will influence our decisions around the use / deployment of resources.
Three levels of priority have been agreed as below:
| Priority | Description |
| Priority 1 Services | These key services are essential priority and are required to be maintained at full capacity. Normal staffing numbers and skill mix will be maintained. This includes 24/7 inpatient services, supported living houses, urgent access / crisis services and key support services which include Switchboard, Estates and Digital. |
| Priority 2 Services | These services need to be maintained but may safely be delivered at a reduced capacity or alternate skill mix. This will be informed by an assessment of service user needs, risk and vulnerability using our agreed clinical RAG rating process. Services may therefore be reduced or consolidated, and some staff redeployed into priority 1 services. |
| Priority 3 Services | These services could be reduced to a minimum level of delivery or could be stepped down entirely. Most staff are therefore likely to be redeployed into priority 1 services (or into priority 2 services as part of a revised skill mix to release other staff to priority 1 services). |
Priority 1 services have been identified as our inpatient wards (excluding respite services) and services that people use to access mental health services in a crisis (CRISS & Section 136, ALPS, Hospital In-reach, Liaison Service, Learning Disability Intensive Support Team, and Older Peoples Intensive Home Treatment Team (crisis and home treatment)). These services also have a high level of reliance on some support services. A full list of services and their priority can be found at Appendix B.
2.6.2 Key risks and mitigations
As part of our winter planning, we have set out the key mitigating actions and monitoring processes for each of our identified key risks as follows:
| Identified Risk | Mitigation | Monitoring |
| High levels of staff unavailability as a result of illness / absence | • Daily monitoring and forecasting of staffing situation and absence • Robust planning, e-rostering and use of temporary staff as necessary • Increase in responsive workforce capacity • Identification of corporate / support staff able to support delivery • Deployment and redeployment process & plans in place • Group established to oversee deployment and staffing • Workforce governance structures in place. |
• Weekly service heat maps reviewed at the Operational Huddle • Escalation through the Strategic Coordination Group (SCG). |
| Changes to national response to Flu/ Covid-19 pandemic requiring further rapid change to service delivery | • Incident Management and IPC arrangements in place and tested; able to resume at pace • Strengthened operational structures in place and well established • Evidence of service ability to respond quickly and flexibly. |
• Service changes overseen and monitored via CSDDG and EWCG • Decision logs maintained to record rationale and objective of change. |
| Significant delays in dementia pathway resulting in high levels of people Clinically Ready for Discharge (CRfD) and bed pressures | • Identified priority with Leeds winter plans • Use of winter monies to focus on potential solutions • Partnership planning and delivery with social care. |
• Performance and activity reports (CRfD and bed occupancy) • Weekly meetings with social care and commissioners • Daily capacity and demand reports. |
| Significant increase in pressure on the acute sector (ED attendances, occupancy and bed pressures) | • Increased capacity in ALPS / Liaison service • Partnership approach with LTHT and system escalation and governance arrangements • ED avoidance assessment area in operation. |
• Daily capacity / demand report • Performance reporting framework – metrics relating to ED and LTHT mental health activity. |
| Severe weather resulting in disruption to services (staffing, access, estates risks such as power outages) | • Business Continuity and Deployment & Redeployment plans in place, supported by strengthened operational management structures • Structures in place to support rapid response • Estates business continuity plans and on-call arrangements • Mutual aid. |
• Escalation to EWCG • Estates, IT & procurement reports via EWCG. |
| Reduced engagement of staff as a result of ongoing pressures and repeated changes | • Health & Wellbeing and staff support interventions, leadership packs and oversight group • Mental Health and Wellbeing hub • Enhanced and regular comms and engagement forums (including CEO open sessions) • Local team / service line communication structures, briefings and virtual staff meetings • Individualised Wellbeing risk assessments and managerial relationships. |
• Health & Wellbeing governance structures and Workforce committee • HR metrics • Evaluation reports • Staff survey. |
| Increased pressure on access services and reduced community capacity resulting in increased admission and Out of Area placements and disruption to pathways | • Increased capacity in clinical triage, CRISS and crisis house • CAU remodelled to provide short term assessment with CRISS • Daily capacity reviews and regular partnership meetings • Assertive monitoring of Out of Area placements (case manager) |
• Daily monitoring and reporting (OPEL) • Weekly capacity system meeting with partners |
The risks identified above have been captured in the Strategic Coordination Group’s risk register and will be monitored via that group with risk being a standing agenda item.
3. Winter Management Arrangements
3.1 Current Service Provision and Prioritisation
Services have continued to adapt their method of delivery over the past couple of years, with our services now operating a hybrid model of face-to-face and virtual clinical activity. Service leaders have supported this by developing detailed updated working instructions so that staff have clarity to support their work. Where services have identified issues in relation to backlog and/or waiting lists, work has been undertaken to plan to address these issues, supported where possible by detailed activity plans.
We continue to experience operational pressures across services, especially in terms of increased demand, recovering backlogs of treatment and care, and ongoing constraints in how we can deliver care. This occurs in the context of significant wider system pressures, which are already evident as we move into winter.
Throughout 2025 thus far we have seen disruption due to Collective Action taken by GPs resulting in them declining to undertake work on behalf of secondary care. We have seen some impact on our service users; however, we have been able to respond and to put in place the necessary arrangements to ensure their needs are met. There are ongoing negotiations between the GPs and ICB, with the Trust being represented at these meetings by several Heads of Operations.
We are anticipating further Industrial Action (IA) by Junior Doctors and Consultants later this year leading into winter. The BMA has balloted its members to obtain a mandate for IA for 6 months from July 2025, which would enable them to strike at any time until January 2026. We have established a Strategic Coordination Group (SCG) to plan for and manage any IA to coordinate and maintain services during this period.
Our workforce availability, wellbeing and resilience is key in maintaining our ambition for minimal disruption to service delivery throughout the winter, therefore this is where much of our effort and support will be focused. We now have well established contingency arrangements and measures to maintain staffing availability and also to maintain delivery of our access, crisis and inpatient priority services.
These pressures will be managed through the Heads of Service with an escalation route to the SCG during normal working hours. Outside of these hours we have a robust on-call system with three tiers of escalation including a Duty Manager, CSM on call (Tactical) and Director (Strategic) who will then report any issues into the SCG on the next working day.
3.2 Activity and Performance Management
During 2025 services have continued to receive and review activity data, with increasing access to performance dashboards. We have re-established more regular formalised governance arrangements relating to performance and activity via our Care Services Delivery and Development Group (CSDDG), led by the Chief Operating Officer and through the development of the Care Services Performance Group led by the Deputy Director of Operations. We have also maintained our ‘heat map’ approach for all service lines which is reviewed regularly via a weekly Operational Huddle and highlights areas of particular concern or challenge to maintaining service delivery and business continuity.
We will continue to maintain and improve our response times to referrals into our services as normal throughout winter. This may be impacted by any changes to our service delivery because of the response required to support our priority services as part of the Business Continuity approach to maintaining services. Where this is the case, the services impacted will continue to deliver a reduced service and develop recovery plans to demonstrate how they will recover to the position prior to any changes being made following a further EHIA. This will be monitored through our Care Services Performance Group which is reported to the Board as part of the Chief Operating Officer’s report on a bi-monthly basis. Our activity and performance will continue to be monitored through a monthly submission to ICB Commissioners and completion of mandated NHS England returns for specialised commissioned services.
3.3 Service Line Assurance Report
As part of our Winter Plan, each service line is required to complete and provide an assurance template that confirms the service line has adequate confidence in their processes and planning in relation to:
- Staffing (planning, cover arrangements and disruption mitigation)
- Surge and Capacity (service response to manage surge and increased demand)
- Severe winter weather (ability to operate within significant periods of adverse weather)
- Outbreaks (ability to manage Covid-19 and Flu outbreaks).
This detailed assurance (with plans for additional actions and assurance as required) forms part of our comprehensive winter / emergency planning approach and ensures effective oversight and support for our services.
The report template is attached at Appendix C.
3.4 System level winter arrangements
To support the oversight and management of risks over last winter, the new Operational Pressures Escalation Level (OPEL) framework was introduced. This OPEL framework will continue to be integral to the monitoring and management of the risks resulting throughout winter 2025/26. The West Yorkshire System Coordination Centre (SCC) continues to monitor performance and responsiveness to ensure we support patient access. The SCC is a central co-ordination service to providers of care across the ICB footprint, with the aim to support patient access to the safest and best quality of care possible.
The Leeds health and care system will continue to maintain a system OPEL that reflects the wider system pressure and supports system leaders to balance risks. There is an established governance structure in place to manage these pressures over winter and there is a clear process for escalating system calls as detailed in iagram 2 below:
Diagram 2

Within the Same Day Response Programme, priority mental health actions relate to:
- Increasing capacity within our CRISS service to ensure timely access to mental health services in a crisis
- Reducing the number of service users waiting in Emergency Departments over 24 hours for a mental health bed
- Ensuring smooth transition from points of access into mental health crisis services
- Increasing capacity of third sector crisis support services, promoting access alternatives to Emergency Departments.
Within the System Flow Programme, we have specific priority actions relating to:
- Ensuring an effective end-to-end process review for people with complex dementia (both within the Mount and within LTHT), aiming to reduce the number of people in beds with complex dementia who no longer require a hospital bed
- Promoting and embedding implementation of pathways for younger people with mental health and housing needs, who no longer require a hospital admission.
4. Winter staffing
Having sufficient experienced staff on duty is a major asset in mitigating disruption, and a key potential risk to delivery throughout the winter period. Staffing pressures have however remained constant (at varying degrees) throughout 2024/25. Service lines monitor their staffing arrangements and any capacity issues that need addressing are escalated on a regular basis so they can be addressed in a timely fashion.
Winter staffing rotas are not done in advance through the whole winter. However, all teams are frequently reviewing rosters and planning in line with our electronic roster guidelines which ensure rosters are managed effectively and any shortfall can be identified and mitigations put in place.
We continue to see in-year variation regarding the taking of annual leave. These have tended to be through the height of summer, over the Christmas period and the end of the financial year. We know that increased rates of leave create pressure for the remaining workforce and reduces the responsiveness. At this stage of the year, we are seeing the usual trend in use of annual leave albeit at a reduced level (see Graph 13). We will continue to monitor this and put plans in place to start planning for the periods where we see increased use.
To maintain effective working, we operate with an optimal annual leave rate of between 11% and 17% throughout the year. We will take a proactive approach to try to maintain annual leave within these parameters and will ensure our priority services are fully staffed and operational to meet any increased demand. We will also ensure we have sufficient resilience in our system particularly our crisis, home treatment and liaison psychiatry services.
Graph 13
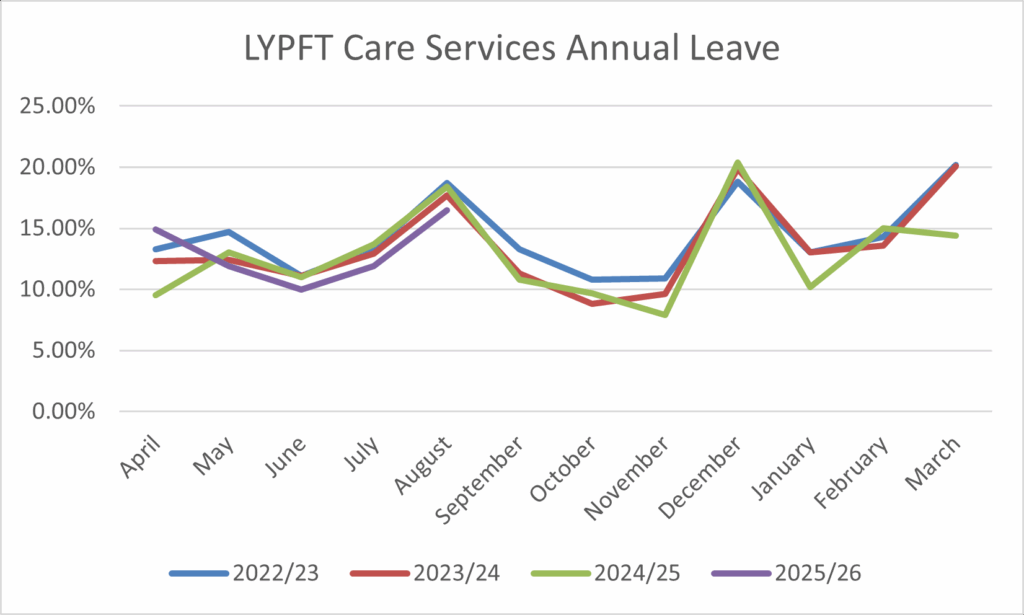
4.1 Maintaining Safe Staffing
Having sufficient experienced staff on duty is key to mitigating disruption to delivery throughout the winter period.
During the initial stages of Covid-19, the Trust developed a formalised approach to the deployment and redeployment of staff to maintain minimum safe staffing levels, particularly within the agreed priority services. This was revised following a period of review and feedback from staff, as well as a formal evaluation of effectiveness and impact. Our current Deployment & Redeployment process can be found at Appendix D.
Operational staffing arrangements, staffing pressures and the forecast staffing position across care services are reviewed within each of the service line management meetings, reporting to the CSDDG and linking closely to the Trust’s governance structures relating to workforce planning, recruitment and retention.
Staffing pressures have however remained constant (at varying degrees) throughout 2025. This is due to periods of increased unavailability of staff, high rates of vacancies and some sustained levels of demand for additional staff in priority services because of service user presentation and acuity. These are now predominantly dealt with through ‘internal’ deployment of staff within the service line (for example, practice development staff or senior clinical staff working directly within the clinical settings), cancelling non-essential activities, or through the ‘day-to-day’ deployment of staff from one area to another (as set out in the Trust’s Staffing Escalation Protocol).
Services will enact their business continuity plans and associated OPEL actions where the triggering staffing levels identified in their Business Continuity Plan are reached, or where levels of activity and demand create pressures that result in an increasing OPEL position. If a business continuity incident is declared, the appropriate ICB will be informed as per EPRR guidance. This would also include reviewing the CSM on call arrangements with a view to Heads of Operations moving to 7-day working as we did during the Covid-19 Pandemic.
These will include:
• Escalation internally and externally with partners (via system Silver)
• ‘Internal’ redeployment of staff across service line to meet priority service needs
• Deployment of clinically qualified senior staff into direct clinical roles
• Cancelling of non-priority activities, study leave and ‘ad-hoc’ annual leave.
• Facilitate early discharge (utilising CRISS / IHTT for increased home support)
• Use of non-designated ward / bed space (such as de-escalation areas or additional bed capacity) to create capacity.
• Review of clinical activity across all service lines with reduction to release capacity and maintain priority and essential services
• Use of volunteers from other services who have identified a willingness to be redeployed to priority services when required
• Use of administrative / corporate support staff within care services.
• Consider step down of services in non-priority category (supported by impact and risk assessments and mitigation)
• Implement formal redeployment processes across care services and corporate support services to maintain minimum staffing and the delivery of priority services.
4.2 Focus on Workforce
The NHS People Plan clearly set out the national aims and objectives in relation to our workforce moving forward, with a key focus on four areas:
- Looking after our people– with quality health and wellbeing support for everyone
- Belonging in the NHS– with a particular focus on tackling inequalities and the discrimination that some staff face
- New ways of working and delivering care – making effective use of the full range of our people’s skills and experience
- Growing for the future– how we recruit and keep our people, and welcome back colleagues who want to return.
These areas have influenced and been reflected in our ways of working over the last four years and are reflected within our 2025/26 Winter Plan. Our Trust People Plan which was first published in 2021, has been recently reviewed and updated for 2024-27, following extensive staff engagement. This outlines the objectives and action plans aligned with the national People Plan, ensuring that over the next three years we can be confident that we are focusing our efforts in areas that will make the greatest impact.
Workforce is identified as the key risk to every aspect of our system and local winter plans. In relation to the Winter Plan, there is a specific focus on two key areas: staff health and wellbeing; and different ways of working to most effectively deploy staff to meet service user need and maintain the continuity of our priority services. Our plans very much reflect the most recent national NHS guidance and advice in relation to preparation for winter 2025/26 and demand surge, which focuses on:
- Provision of health and wellbeing support
- Focus on flu vaccination
- Effective forward planning of deployment and rosters
- Recruitment and retention initiatives to grow, develop and upskill the workforce
- Promotion of resilience and increased flexible working arrangements.
4.3 Staff wellbeing
The wellbeing of our staff is our priority, and the objectives set out in Our People Plan ensures staff are being supported to feel safe, healthy and well both physically and psychologically. The Wellbeing and Attendance Management Group meets monthly and oversees and coordinates our approach to staff wellbeing reporting through the People and Organisational Development (POD) governance, and bimonthly to our Wellbeing Guardian (Non-Executive Director) at the Workforce Committee.
In addition to the annual Performance Development Review (PDR) for individuals, regular Wellbeing Assessments should be undertaken. Wellbeing Assessments are further supported by the Wellbeing Agreement which is completed by staff supported by HR who are seeking further health and wellbeing support because of a change in their health and wellbeing and/or the diagnosis of a disability, a long-term condition or illness. It can also be following a change to a pre-existing condition.
The health and wellbeing offer to staff is regularly communicated through a monthly wellbeing focus in the Trustwide newsletter and through our Staffnet pages. This provision includes rapid access to services such as stress, anxiety and burnout therapy, counselling, physiotherapy, cognitive behaviour therapy (CBT) and our occupational health service.
The Health and Wellbeing Team is available to support any teams or service that are under pressure through programmes such as our Critical Incident Staff Support Pathway (CRiSSP), Ward Wellbeing Buddies and Health and Wellbeing Champion network.
In addition, we play an active role in the Leeds One Workforce Programme (a set of continuing collaborative projects relating to workforce support and development) and the West Yorkshire staff health and wellbeing hub. The Thrive @ Work programme supports employees working in a health and care organisation in Leeds with support services, including Health and Work coaching service, Leeds workplace adjustment service, Mental Health fast track support, Musculoskeletal (MSK) support, support with career choices and transition.
5. Supporting the health of our people and patients over the winter
5.1 Previous Seasonal Vaccination Campaign uptake
Over the past three years we have seen a decline in the uptake of Flu and Covid-19 vaccines by eligible staff (see Graph 14). The reasons for this are unclear; however, one reason could be because of vaccine fatigue. There is a national emphasis to increase the rates of vaccine uptake this year. Whilst there is no national target set we are working to a goal of 100% of staff being offered the vaccine with the aim of improving on the previous year’s uptake by 5%. Section 5.2 sets out the Trust’s strategy for the vaccination programme for winter 2025/26.
Graph 14
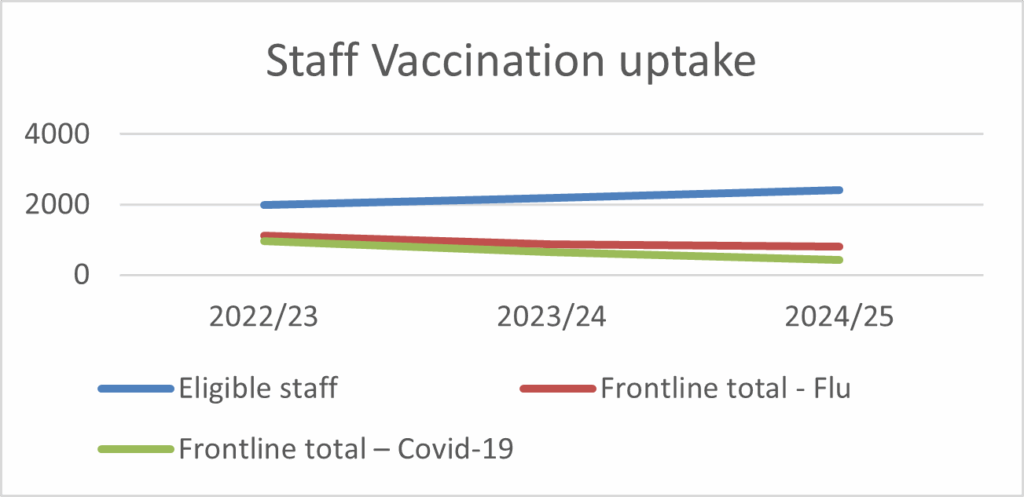
During the winter period we see an increase in staff absence rates, and this has been consistent over the past three years (see Graph 15), with the overall absence rate fluctuating between 5.5% and 6.5%. We also see a seasonal increase of absence due to respiratory related infections; however, these remain reasonably low, ranging from 0.5% and 1.5% of our total workforce. Based on the previous year’s absence rates we anticipate this will be the trend we will see through this next winter. Plans are in place to support and manage sickness absence across the organisation and an overall reduction is one of the Trust’s priorities for this year.
Graph 15

5.2 Autumn/winter 2025-26 Vaccination Plan
We started planning for this year’s vaccination programme in June 2025, which will see it commence earlier than previous years in September. As a result of anticipated early delivery of seasonal flu vaccines, the Infection Prevention and Control Team (IPCT) will start conducting ad-hoc drop-in visits onto inpatient wards from mid-September. The aim will be to offer vaccine at the earliest opportunity to all staff and service users, who have had the vaccine prescribed following medics assessments.
NHSE have circulated the eligible cohort for the upcoming Autumn Covid-19 vaccination campaign. We will only be offering vaccine to eligible service users until the 19 December 2025. Health and social care workers are not included in the eligibility criteria for Covid-19. Co-administration of flu and Covid-19 vaccine will be offered to service users.
Vaccination will be offered in England in autumn 2025 to:
- Adults aged 75 years and over
- Residents in a care home for older adults
- Individuals aged 6 months and over who are immunosuppressed, as defined in tables 3 and 4 of the COVID-19 chapterof the UK Health Security Agency (UKHSA) Green Book on immunisation against infectious disease.
To maximise uptake and visibility, the focus will be more on drop-in vaccination visits onto inpatient areas and less static clinics.
The campaign plan will include,
- Drop-in sessions from September daily to inpatient wards offering flu vaccine to service users and staff and Covid-19 vaccines to anyone that is eligible (this will be communicated to clinical teams to ensure cooperation and to ensure service users are assessed for vaccine eligibility ahead of the sessions).
- 1 static clinic split into two on different sites each working day (for example 8.30 am till 12 noon at St Marys Hospital Site then 1.30 pm till 4 pm at the Becklin Centre) The drop-in sessions will be publicised via an all staff Trustwide Communications email on a weekly basis.
- Registered Nurses and Registered Nursing Associates in inpatient areas who are peer to peer vaccinators offering the flu vaccine to staff working in that area.
- The IPC team will facilitate vaccination clinics within Leeds from October till December. From January till the end of March, the IPC team will do walk-around visits onto wards to offer the vaccine to those who have not been vaccinated. This will include obtaining signed consent forms from staff who have had the vaccine elsewhere and those who choose to opt out. This is to ensure we can evidence 100% offer to all frontline staff.
- Registered staff on the wards will vaccinate service users with the flu vaccine as soon as possible to ensure early protection.
- The IPC Lead Nurse/ Vaccination Campaign Lead will record monthly frontline vaccination uptake figures on ImmForm, the UKSHA data collection system. A report of uptake figures will also be shared at the IPC Committee and with the Nursing and Professions Directorate.
The IPCT will ensure records of staff and service user vaccine uptake is recorded on RAVS (Record a Vaccine Service) previously known as NIVS (National Immunisation Vaccination Service).
5.2.1 Publicising the campaign
The campaign will be simple, visible, and rewarding. We’re framing vaccination as an act of healthcare heroism: “be a flu fighter to protect yourself, colleagues, and patients”. We’ve conducted photo shoots in clinical areas, which have been well received, to develop our visual concepts. Posters will be printed featuring colleagues across the Trust under the theme “Flu Fighters”, to be displayed across key Trust locations / inpatient wards. Stickers and goody bags are in production to make the experience positive and rewarding.
We’re also using social influence, celebrating uptake across wards in order to create positive peer pressure to drive participation and sharing their “why I got jabbed” stories. Managers are being supported to emphasise the role of vaccination in keeping wards staffed and safe over winter, addressing key areas of concern including myths and misinformation.
We’ll be promoting a clear timetable of dates and locations, alongside guidance for staff who prefer to use local clinics. We’re also regularly reminding staff to complete the “Flu Form”, to give consent, state if they’ve received their vaccine elsewhere, or if they are not interested, to keep our data accurate.
5.3 Fit Testing
NHS England is mandating that ‘Fit Testing’ has taken place for all relevant staff groups. The IPCT will offer Fit Testing in clinical areas at the request of the Team Managers. In addition, all eligible staff will be provided with Fit Testing during any relevant mandatory training sessions. Team managers will be asked to provide the IPCT with a list of exempt staff who cannot be Fit Tested due to health or other reasons. Records of staff completing Fit Testing will be held on ESR.
5.4 Outbreak Management
We have seen the rates of respiratory related infections in our service user population reduce over the winter months for the past three years (see Graph 16). We have also seen a reduction in the number of outbreaks reported (see Graph 17). In addition to this we have seen the average duration of the outbreak reducing from 12 days for the 2022/23 period to 10 days for subsequent periods.
Graph 16
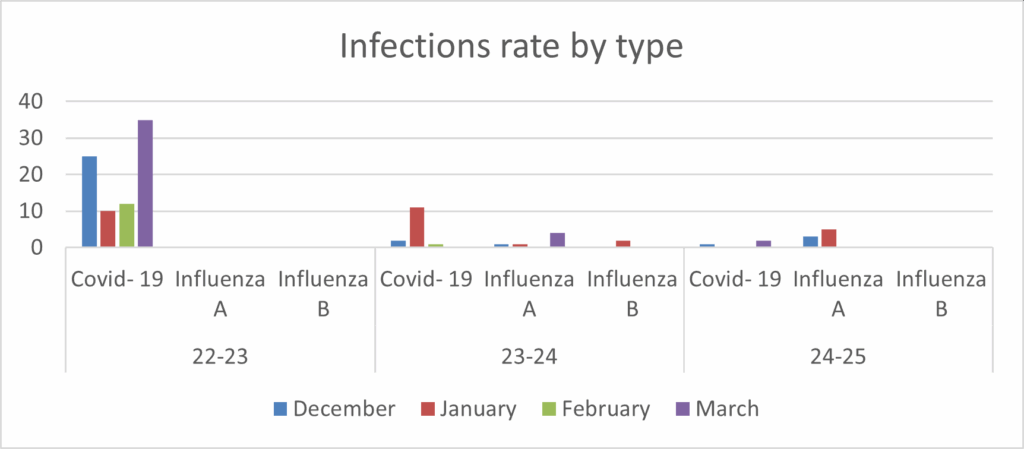
Graph 17

We will continue to follow previous year’s approach to outbreak management as follows:
- During working hours, the IPC team will stand up outbreak management meetings where an outbreak has been identified of any causative organism
- Once IPC have been notified of two or more service users presenting with symptoms, IPC response time should be within 2 hours Monday to Friday 8 am till 4 pm
- An outbreak meeting will be held which will inform clinicians on the ward of the standard infection precautions they should implement to safeguard others
- From 8 am till 5 pm Monday to Friday, the IPC team will provide a telephone advisory service and respond to staff/service queries
- The Outbreak and Countermeasures Plan sets out the Trust response to an outbreak on Trust premises and in the community.
6. Addressing Health Inequalities
Adverse cold weather can put people already experiencing health inequalities at greater risk of ill-health and even death, primarily because it increases the probability of complications from existing disease, and of injury due to falls.
There are a number of ways we can support the people we care for to reduce the risks associated with exposure to adverse cold weather including:
- Knowing who is at risk
- Being alerted to increased cardiovascular, respiratory and other complications from cold exposure
- Adapting individual care plans to respond to adverse cold weather
- Promoting vaccination for those eligible to reduce risks from Covid-19 and flu
- Having action plans in place tailored to the local context
- Signposting people to sources of support for housing, energy billsand other needs as appropriate, including specific support for those on low incomes.
We know fuel poverty is a long-standing health issue: the impact of cold housing on health and the stresses brought on by living in fuel poverty have been recognised for decades by researchers, medical professionals and policy makers alike. Fuel poverty is a longstanding council priority and aligns strongly with the Leeds Best City aim of tackling poverty and reducing inequalities.
Any increase in fuel poverty is concerning, but this issue has recently been amplified due to increases to energy bills and a rise in the cost of living more generally. Councils have launched schemes to help residents cut energy bills and homeowners, renters, and landlords of properties without gas central heating can now get energy saving green measures installed free of charge or at a significant discount, thanks to a new Council scheme.
Below are some resources available to service users and staff to help deal with the winter pressures people may experience:
There are many organisations that offer free, impartial and confidential help and advice with all types of debt including rent arrears, council tax and utilities. Many also offer help with other money problems such as benefit issues and budgeting and can be found at Energy, utility and household bills.
Staff working with people experiencing fuel or poverty emergency or crisis, can apply for support with food, energy and essential household items through the Councils Local Welfare Support Scheme. The Leeds City Council one can be found on Local Welfare Support Scheme, City of York Council can be found on Energy grants for homes not heated by mains gas.
Staff can also access Supporting vulnerable people before and during cold weather: healthcare professionals with action cards. (There are also the same for hot weather).
7. EPPR response
7.1 Winter Coordination
7.1.1 Strategic Coordination Group
To manage winter pressures, risks and any resultant disruption we will convene the Strategic Coordination Group. This executive-led group comprises a multi-disciplinary team of senior staff and has the remit to mitigate the risk of disruption from a wide range of factors ranging from weather to capacity, demand, and flow to infectious outbreaks. The group is supported by a Tactical Coordination Group charged with minimising environmental and weather-related impacts on Trust services.
The Strategic Coordination Group will convene on the 22nd September 2025 and will run until the end of March 2026 with an assessment on the appropriateness of standing down the group to be made in late March 2026. The group reports to the Trust’s Executive Management Team.
7.1.2 Tactical Coordination Group
The Tactical Coordination Group will operate from October 2025 to coordinate all work to mitigate potential winter disruptions. The membership of the group includes:
- EPRR staff
- Estates and Facilities
- Operational Management
- Communications
- Physical Health
- Membership from Mitie and NHS Property Services.
Its role covers adverse weather response, power outage mitigation, disruption to other utilities and response to disruptive snow regarding site access. The group will report to the Trust’s executive-led Strategic Coordination Group.
7.2 Adverse weather
The Trust has an Adverse Weather Plan that has been developed to manage adverse weather conditions over the winter period. The plan contains full details of the Trust’s risk assessment, impact assessment and mitigation around disruption from adverse weather.
The Trust’s EPRR team is registered to receive alerts regarding adverse weather from the Met Office, and flooding information and risks from the Environment Agency.
The Adverse Weather plan describes the process for communications with staff and when all-user e-mail notifications will take place so that services can consult their business continuity actions in preparation for potential bad weather, for example, going to standby with flood defences at a site at high risk of flooding. Requests for these alerts are to be made via the Trust Communications Team:
- In hours: A request to be made by phone to the duty comms officer central number: 0113 85 55989.
- Out of hours: If the Director on call (Strategic Commander) declares a critical or major incident out of office hours, they can request out of hours comms support by calling 07534 907491.
For significant threats, amber or red warnings, the Trust would invoke organisational business continuity arrangements aimed at utilising resources to maintain critical clinical and organisational activities.
Incident coordination would also be an option that would be considered for managing widescale disruption and has been used in previous winters to manage disruptive snow events. Incident coordination would follow the principles set out in the Trust’s Emergency Incident Response Plan.
7.3 Other winter risks
7.3.1 Power disruption
Winter brings with it increased risks to power distribution based on both the impact of storms and supply sided shortages first experienced in winter 2022/23 with a risk to gas and oil supplies caused by the Ukraine conflict and UK gas storage limitations.
Many of the same factors exist in winter 2025/26 as in previous years, hence the Trust will carry out work to boost resilience around potential outages. As part of this:
- The Trust will implement a series of black start tests, simulating a power cut, testing the back-up generators and their control system’s ability to detect the outage and then activate and power the building
- Emergency lighting equipment will be checked to ensure it is in place and is still effective. This includes checking ward stocks of torches and LED safety lights issued to services across the Trust
- Communication equipment checking will be requested for all in patient areas, these are ward business continuity mobile phones.
7.3.2 Maintaining access to Trust sites.
The Trust’s sites are covered by three providers of facilities services: Trust owned and leased sites provided by Trust Estates staff; Leeds PFI sites provided by Mitie; and York sites provided by NHS Property Services. All three providers have in place advance warning arrangements via met office alerting, supplemented by EPRR issuing warnings.
On receipt of a snow or ice warning the providers will mobilise snow clearing and gritting resources to maintain access to sites including an out of hours response.
7.3.3 Equipment shortages
During the summer of 2025 we were notified that Nottingham Rehab Limited, NRS Healthcare Limited, and the Complete Care Shop, went into liquidation on 1 August 2025. These companies are major suppliers to the NHS, local authorities and to individual service users for equipment to support care and activities of daily living; everything from protective gloves to beds, and many things in between. Concerns have been raised as to the impact any equipment shortage would have on our ability to discharge service users who may rely on additional aids to support discharge.
Whilst NRS Healthcare Limited is one of the largest suppliers to the NHS, the Trust has good alternative suppliers already in place and we are confident we will not be significantly affected by this announcement. However, to have oversight on this issue and to respond to any further challenges we have established a Tactical Coordination Group which will maintain this oversight. The group membership includes the EPRR Lead, Operational Managers, clinicians and procurement colleagues from all areas of the Trust that may be impacted by this announcement. This group currently reports into the Strategic Coordination Group, established for Industrial Action. As we enter winter and establish the Strategic Coordination Group we will report any issues there as well.
We have shared the following key messages across the Trust:
- Continue to order equipment through the normal purchasing processes via our Procurement Team who already have good quality suppliers in place, and who are able to source alternatives where necessary and appropriate
- Not to order any goods or services outside of existing processes without consulting either procurement or professional leads
- Avoid any unnecessary prescription of equipment and ensure the most effective use of equipment already available, including seeking the return of unused items, as there will be pressures in the national supply chain during the fallout from this announcement.
8. Conclusion
As discussed throughout this plan, we continue to see pressure across our services, particularly our acute inpatient and liaison services, throughout the year. Whilst we have plans in place to work to improve the position, we expect this to continue into winter and beyond.
Winter brings the added pressures from across the wider system, nowhere more so than in our Acute Hospital provider, which results in added challenges to the delivery of mental health services. Working with the Integrated Care Board and other healthcare provider partners, including the VCSE, we will ensure that disruption is kept to a minimum for the people we provide services for.
Joanna Forster Adams
Chief Operating Officer
Contributions by:
- Mark Dodd: Deputy Director of Operations
- Cath Hill: Head of Operational Governance
- Sam Grundy: Head of EPRR
- Gugu Ncube-Mpofu: Lead Infection Prevention and Control Nurse Specialist
- Eve Townsley: Head of Operations for Liaison and Perinatal Services
- Ian Burgess: Senior Information Manager
- Sophie Valinakis: Head of Health Equity
- Laura McDonagh: Head of Operations for Acute Services
- Warren Duffy: Deputy Director of Estates and Facilities
- Holly Tetley: Associate Director of Employment
Glossary
| Term | Explanation |
| Business Continuity | The capability of the organisation to continue delivery of products or services at acceptable predefined levels following a disruptive incident. |
| Business continuity incident | An event or occurrence that disrupts, or might disrupt, an organisation’s normal service delivery, to below acceptable pre-defined levels. This would require special arrangements to be put in place until services can return to an acceptable level. Examples include surge in demand requiring temporary re-deployment of resources within the organisation, breakdown of utilities, significant equipment failure or hospital acquired infections. There may also be impacts from wider issues such as supply chain disruption or provider failure. |
| Command and control (and communication) | Often referred to as C3. The exercise of vested authority through means of communications and the management of available assets and capabilities, in order to achieve defined objectives. |
| Critical incident | A critical incident is any localised incident where the level of disruption results in the organisation temporarily or permanently losing its ability to deliver critical services, patients may have been harmed or the environment is not safe requiring special measures and support from other agencies, to restore normal operating functions. |
| EPRR | This refers to Emergency Preparedness, Resilience and Response – this term covers all aspects of responding to emergency incidents and disruptive events in the NHS. |
| Mitigation | Measures taken to reduce an undesired consequence |
| Mutual aid agreement | Pre-arranged understanding between two or more entities to render assistance to each other |
| OPEL | Operating Pressures Escalatory Limits – this is the NHS England Framework governing how health providers reflect their position regarding capacity, demand and flow and the necessary actions to take to try to alleviate these pressures. |
| SiTRep | Situation Report – a teleconference or report detailing the current situation affecting a service, department or site. This is used as a basis to formulate action to manage the incident or problem. |
Appendix A
| Initial EHIA Screening Questions: | Yes or No |
| 1. Are you reviewing a policy, procedure or are your services due for review or introducing new changes? | No |
| 2. Are you establishing a new policy, procedure, or developing a new service? | No |
| 3. Could the policy / service change or the way in which it is carried out have a negative impact on people with a particular protected characteristic? For example, does it put a particular group at a disadvantage on the grounds of age, disability, sex, ethnicity, gender reassignment, marriage and civil partnership, pregnancy and maternity, religion or belief, and sexual orientation equality? | No |
| 4. Could the policy / service change or the way in which it is carried out have a negative impact on relations between different groups? | No |
| 5. Is the negative impact, if any, unavoidable? Could it be considered to be unlawful discrimination? Can it be justified by the aims and importance of the policy/service? Are there other ways in which the Trust’s aims can be achieved without causing a negative impact on some diverse groups? | No |
| 6. Could taking particular measures, reduce the negative impact? | No |
| 7. Is further research or consultation necessary? Would this research be proportionate to the importance of the policy/service/function? Is it likely to lead to a different outcome? | No |
Appendix B: Service Priority Categorisation
Priority Services
| Service / Area | Operational Notes |
| CRISS Older Peoples IHTT LD Intensive Support Team ALPS and LTHT Liaison Inreach Section 136 suite |
All crisis / urgent access services |
| Acute Wards and PICU CAU Mount wards Asket Wards CYP inpatient wards (Mill Lodge and Red Kite View) Mother and Baby Unit YCED (Ward 6) Complex Rehab (Ward 5) Forensic Wards 2 and 3 Woodlands Square Supported Living |
Inpatient services and Supported Living Houses – maintain 24/7 Some reduction in full MDT availability in some teams, which will be managed by cross cover or redeployment (depending on requirements) Minimum staffing requirements being reviewed and confirmed in partnership with nursing directorate |
| NICPM | Maintain as a priority ward. |
Maintain but can reduce / redeploy some staff
| Service / Area | Operational Notes |
| CMHTs CLDTs Assertive Outreach Community R&R CONNECT community team Community Forensic Team Community Perinatal Deaf CAMHS Physical Health Team Care Homes Team Recovery College (telephone & online support) Forward Leeds (Addictions) PD Network LADS and ADHD Gender service Gambling service Chronic Fatigue & Liaison Outpatients Psychosexual medicine Offender PD services OpCourage Enhanced Pathway Team OpCourage Core Pathway Team |
These services can all operate currently on a reduced number of staff but have a requirement to maintain some access and an active caseload, including direct contact (including some face-to-face contact) with some service users. All service users have been RAG rated, and this informs us of the required capacity and skill mix for the team. Some staff are therefore available for redeployment from these teams. |
Could step down
| Service / Area | Operational Notes |
| LD Involvement Team PD Pathway Development Service MH Primary Care |
These services can be closed to new referrals and stopped down, with only emergency contact cover in place. Priority cases would come via crisis or liaison where necessary. |
Essential Support Services
These support services have been identified as being critical to the ongoing delivery of care services:
- Information Technology – provision of:
- Care Director
- EPMA
- E-mail system.
- Shared folders and wide area network
- Access to NHS spine apps and Leeds Care Record
- Big Hand
- Pharmacy – provision of medication, advice and support to clinicians
- Estates – provision of:
- Hard and soft FM at owned and leased sites
- Soft FM at NHS PS Sites
- Liaison with Landlords, NHS PS and the SPV/ Mitie
- Workforce Systems
- E roster
- ESR
- Bank systems
- Procurement – provision of:
- Clinical consumables
- Bill payments for medical equipment
- Consumables, food, drink etc for inpatients
- IPC- advice and response to outbreaks, pandemics, and advice in a HAZMAT/CBRN incident
- Switchboard – Maintaining telephone communications across the Trust
Appendix C: Winter Planning Assurance 2025-26
Introduction
The questions below are focussed on the key resilience principles that need management consideration. After brief, a brief narrative can you RAG rate your assessed level of preparedness.
1. Staffing – do you have effective plans in place to mitigate disruption caused by reduced workforce, annual leave, and the Christmas holiday period?
RAG assurance rating? Red, Amber or Green.
2. Surge and capacity – have you assessed the effectiveness of your plans to manage surge and increased capacity during the winter? For services that interface with other providers have you assessed likely impact on work from these providers facing surge?
RAG assurance rating? Red, Amber or Green.
3. Severe winter weather – assessment of the services ability to continue to operate faced with significant periods of snow/ ice.
RAG assurance rating? Red, Amber or Green.
4. Outbreaks –what is your assessment of your services ability to manage outbreaks in teams and on wards.
RAG assurance rating? Red, Amber or Green.
5. Risks to escalate.
Appendix D: Staffing escalation and deployment protocol
The purpose of this document is to provide guidance on the daily management of the ward ensuring the optimal staffing levels are met which meet the patients’ needs as determined by risk and level of acuity and dependency.
When planned staffing levels are insufficient to meet current patient need, the following principles within the flowchart should be applied. This will enable clinical areas to identify and deploy resources to maintain safety where necessary.
Effective escalation of staffing shortfalls supports timely interventions to resolve issues to ensure a safe environment is maintained for the patient in addition to the health, safety and wellbeing of the staff members on duty.
This protocol should be applied in situations where the staffing level is insufficient within an inpatient ward/unit and applied alongside ‘principles of deployment’.
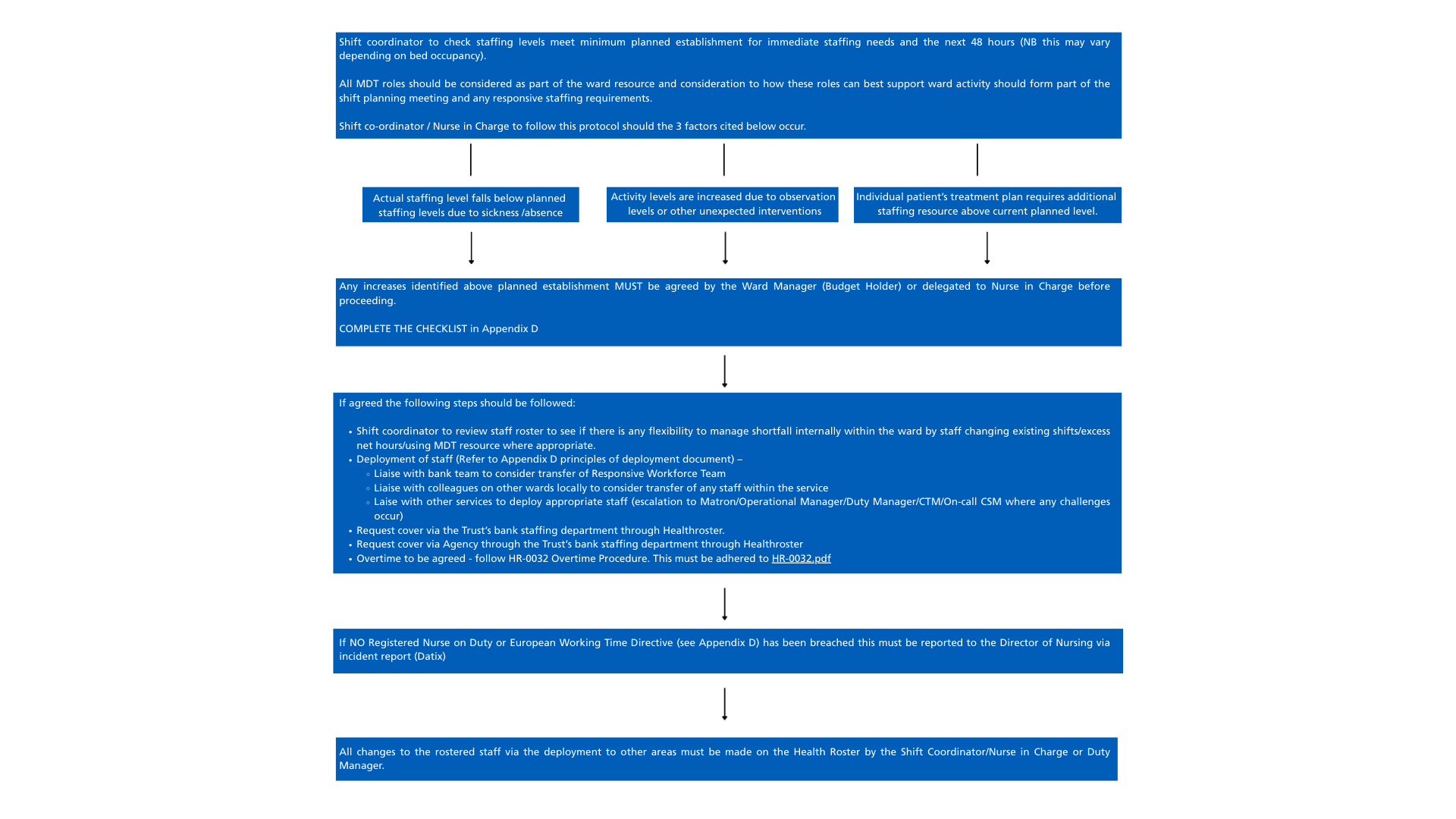
Appendix D: Staffing Escalation and Deployment Protocol Flowchart The flowchart outlines the steps for shift coordinators or nurses in charge when staffing levels fall below planned levels, activity increases, or individual patient needs require extra staff. Key steps include: Checking current and next 48-hour staffing against minimum requirements. Considering all MDT roles for ward support. Completing the Appendix D checklist. Reviewing the staff roster for internal flexibility. Deploying staff per deployment principles. Liaising with Bank partners for additional staff. Consulting with senior staff if challenges arise. Requesting cover via Bank Trust portal or Agency through NHSP. Following overtime procedures if needed. Reporting breaches of Registered Nurse coverage or Working Time Directive. Recording all redeployments in Health Roster. All increases above planned staffing must be agreed by the Ward Manager or delegated Nurse in Charge.
Appendix D/1: Checklist for Safer Staffing
Name of ward or service:
Date:
Shift:
1. Potential staffing shortage identified on unit – reason identified as:
- Vacancy
- Sickness absence
- Special Leave
- Study Leave
- Maternity Leave
- Annual Leave
- High Activity
- Other
2. Has consideration been given to all members of the MDT and how they can support ward operation/delivering patient care?)
3. Can the rota be arranged more effectively to provide the necessary staffing?
4. What would be the consequence of not covering the shift/additional duty? (Risk Assessment) Can this be managed?
5. What will additional staff be required to do? Identify particular grade/s, qualifications, skills or experience.
6. Does the full shift need to be covered or if not, what hours specifically need cover?
7. Requests to cover overtime to be agreed – follow HR-0032 Overtime Procedure. This must be adhered to HR-0032
Considered all option: Mark as Yes or No:
- Explore how the MDT on duty can support ward operation/delivering care whilst maintaining profession specific commitments
- Consider changes to the rota/effective rostering/shift swaps
- Has agreement for an additional duty from WM/CTM or delegated Nurse been sought (Name and Role)
- Consider deployment of RWT
- Consider deployment within own service/site
- Consider deployment within other services
- Request bank cover via healthroster
- Request cover agency via healthrotser
- Utilise overtime (overtime procedure check list must be completed
- Have any changes been made on Healthroster
Name:
Designation:
Signature:
Date:
Appendix D/2: Principles of Deployment
Deployment to an area outside of a staff member’s service, the CTM / Operational Manager or Matron (Duty Manager out of hours) ideally should identify and move staff (substantive or bank) who have previously expressed a willingness.
In the circumstances this is a reasonable management instruction and should the person object, an individual conversation should also take place with the CTM or Matron/Operational Manager to explore the concerns, offer support/guidance and confirm that there are no legitimate/reasonable reasons why the member of staff cannot be deployed to the ward/service (such as ill health or specific personal circumstances), and that they have the necessary skills / training to undertake the role. Information & reassurance should be provided in relation to any unique procedure within the specialty and plans on how this will be managed. Any refusal to be moved that is considered unreasonable should be recorded & reported to the relevant Head of Operations.
Principles:
- All services should have information about their service and an induction process (both Bank and Substantive) which will include induction to the environment and be familiar with the fire safety evacuation procedure and other elements of safety pertinent to that area at the beginning of the shift
- The Duty Manager role is a responsive mechanism to support services where there are staff shortages or other issues that require manager oversight. They are not a pro-active mechanism to support teams with their staffing issues in advance of these issues.
- Staff with medical considerations that would prevent them from being redeployed into specific services should have an active (3 months) OH referral in place, which clearly states what restrictions are in place and a compliant wellbeing assessment.
- All staff should be made aware of the nature of critical responses to staffing pressures from a service user-centric position and explanation provided of the real risk to service user care.
- All Duty Managers and Redeployed staff will be supported by the Trust in undertaking risk assessments, deployment decisions and decisions whilst deployed into services.
Operational:
- Ensure that rosters are created, approved, and published in good time (8 weeks in advance is best practice) to create opportunity for Substantive and Temporary Staff to provide cover for vacant duties in advance of working.
- Service Rostering – Review the current shift-by-shift allocation module at a more service-level approach, including a cluster system so wards look at service before redeploying from outside. This helps in three ways:
- Ensures that people’s skills are matched to services.
- Ensures that people are working within services they are familiar with.
- Ensures all colleagues are sighted on the tiered approach, providing assurance of minimal moves out of clusters.
- Each service ensures it has taken all necessary steps to cover shifts within the team, service, and service line structures during normal working hours. No escalation should be made to the Duty Manager during this time. Escalation to the Duty Manager should only occur at the end of the normal day to flag ongoing issues with an identified plan to resolve them.
- Where redeployment of Healthcare staff is required, the Responsive Workforce Team (RWT) should be considered in advance of approaching ward-based staff. The RWT roster is accessible to all managers under Healthroster.
- Where the RWT cannot provide cover, consider the following before redeployment action:
- Does the staff member have:
- Medical Exemption – Under a current OH referral?
- Skills exemption – Not of the appropriate registration or lacking training to provide safe care (e.g., RNLD moving to Mental Health Unit). A brief assessment of skill set should be undertaken.
- Experiential exemption – Are they a preceptee or involved in a recent incident or performance issue that would prohibit moving?
- European Working Time Directive (EWTD): Consider whether moving or extending hours would breach EWTD or impact caring responsibilities. (Warnings of breaches will be visible on the roster.)
- Does the staff member have:
- Where services require longer-term support, consider moving staff into short-term block bookings/placements to avoid concurrent requests.
- Services should capture all movements to improve data integrity and inform decision-making, reducing commitment of both rostering and management teams on safer staffing follow-ups.
Appendix D/3:Working Time Directive
The UK’s Working Time Regulations 1998 lay down the minimum conditions relating to weekly working time, rest entitlements and annual leave in the UK, although UK employees can opt in and out of the provisions relating to the minimum 48-hour working week
LYPFT’s policy and guidance to WTD HR-0046.pdf has been written in question and answer format for simplicity. If you cannot find the answer to a question, please contact your manager or the Human Resources Department who will be pleased to help you.
Appendix E: Mental Health ED Flow Winter 2024-25 Action Cards
System and Operation Actions – System Level
Regional Actions
- Establish and agree local escalation protocols with ICBs for people with 12, 24 and 48 hour waits in EDs.
- Hold oversight of the numbers of people waiting for a MH bed for each ICB across the whole region and report total demand for MH beds on daily national calls.
- Lead on ensuring that MH Discharge Initiatives are in place and support improvement where required.
- Offer support and attendance at ICB MADE to provide a level of independent external challenge.
- Support bed brokerage across the region when requested by ICBs to source MH mutual aid or specialist beds.
- Support resolution of individual provider disputes both within and across regional boundaries to maintain flow.
- Appoint a named lead to support long waits in EDs and an Exec Clinical lead for escalation purposes.
- Seek assurance from clinical leads daily that the person remains in the most appropriate setting whilst awaiting bedded care and escalate as per local protocol.
ICB/ICP Actions
- Establish/maintain cross agency steering group/boards to hold accountability for oversight, with all agencies signed up to an accountability charter
- Monitor specific counts for the numbers and LoS of MH persons in a G&A bed who have no physical reason to be there.
- Actively address the delays in persons with Clinically Ready for Discharge (CRfD) in MH Trusts to improve lost bed days and increase inpatient capacity.
- Undertake MH bedded and non-bedded demand and capacity mapping and housing demand capacity mapping at system level and commission to close gaps.
- Hold oversight of the MH discharge initiatives for all MH Trusts, and support improvement where they require it.
- Ensure stakeholders and partners have shared principles for accessing a health-based place of safety and mental health inpatient care and treatment when those in a MH crisis need it.
- Ensure that protocols are in place that note all actions, including assessment and referral paperwork, that are required for bed allocation are available to prevent delays with admission to onward destination
- Ensure commissioning of MH crisis alternatives, listed on Directory of Services (DoS) and monitor/promote activity in these services.
- Appoint a named lead for >12 hour waits in EDs and an Exec Clinical lead, an LD & A Specialist and a Local Authority Social Care SRO where there is a requirement for escalation purposes.
- Seek daily assurance that the person remains in the best place for their care whilst awaiting bedded care daily from clinical leads and escalate as per local protocol. Develop local escalation protocols for people waiting 12, 24, 48 hours in EDs and undertake daily escalation via SCC calls with regions re long waits in EDs.
- Report total demand for MH beds/wait lists to regional leads daily in line with MH OPEL Framework (but commence prior to OPEL go-live date)
- Escalate cross-border provider disputes to regions to support resolution where all local escalations have been exhausted. Hold details of named MH escalation lead across ICPs to find MH care within person’s locality (where person is out of area).
- Work with Local Authority to source complex social care placements, particularly where there’s a long delay in transfer of care
- Collaborate with system partners and consider shared objective setting to ensure comprehensive planning and support, especially within social care requirements, ensuring Local Authorities to contribute to this to ensure adequate social care provision.
- Negotiate the expedited delivery of social care packages to prevent unnecessary admissions and support prompt discharge.
System and Operation Actions – Trust Level
Acute Trust Actions
- Appoint a named lead for >12 hour waits in EDs support and an Exec Clinical lead for escalation purposes.
- Act on escalation protocols for people waiting 12, 24, 48 hours in EDs.
- Ensure 24/7 core fidelity for Psychiatric Liaison Team (PLT) is in place and escalate where it isn’t.
- Ensure that assessment and referral to PLT happens in a timely way to allow intervention as early as possible
- Ensure that links are established with the ICB lead for learning disability and autism
- Act on protocols for assessment and referrals for onward placement to prevent admission delays
- Ensure that an in-person review for all patients awaiting a mental health bed or review in the acute or community trust (or more frequent if appropriate) is conducted by a Consultant Psychiatrist to ensure appropriate management and to assess if admission is still required or if the person can be discharged or managed at home or in the community.
- Consider development of policies and/or protocols* that support the operational management of flow and decision making in ED with the aim of getting a person to the right place as quickly and as safely as possible.
See example regional approaches on the dedicated FutureNHS page.
Mental Health Trust Actions
- Appoint a named lead for >12 hour waits in EDs support and an Exec Clinical lead for escalation purposes.
- Undertake demand and capacity mapping at trust level and escalate to ICB where there are gaps.
- Act on escalation protocols for people waiting 12, 24, 48 hours in EDs.
- Assess themselves against the MH Discharge Initiatives and develop plans if these are not in place.
- Ensure that links are established with the ICB lead for learning disability and autism and can check if people are on the Dynamic Support Register and have had, or have an urgent C(E)TR
- Ensure 7 day working, to include clinicians with the ability to approve home leave and discharges on the weekend.
- Persons clinically ready for discharge (CRfD) within bed base and waiting for social support should be escalated to ICB and LA Chief Executives daily.
- Conduct an in-person review for all patients awaiting a mental health bed or review in the acute or community trust (or more frequent if appropriate) by a Consultant Psychiatrist to ensure appropriate management and to assess if admission is still required or if the person can be discharged or managed at home or in the community.
- Seek mutual aid from other MH Trusts in the region/ICB before resorting to an OAP.
- Review community teams (general and crisis teams) caseload daily, to assess clinical need to remain on that caseload and step down or reduce contacts if clinically appropriate, creating capacity within those teams.
- Review inpatients daily to see if anyone could be discharged into the community to create capacity within local MH beds.
- Identify vacant beds and consider opening any short-term beds, beds of those who have absconded, beds of those who are due to return from leave the following day/subsequent days or open escalation beds where these can be staffed.
- Lead bed brokerage for all people awaiting a MH bed. Source an OAP or local/mutual aid and if all other options have been exhausted that is best placed for the patient, with a view to repatriation of the person as soon as possible. Escalate to ICB where demand for a bed exceeds capacity, including planned discharges.
- Treatment and discharge planning should commence as soon as a mental health requirement is identified.
- No reduction in clinical priority for a MH bed should be attributed to the person due to any admission to a medical/community ward
Action Cards by Patient Cohort
Children and Young people
Regional Actions
- Support conversations between ICBs and local authorities in sourcing complex combined health & social care placements where there’s a delay in transfer of care, risking a long wait in ED. Escalate to national team as per protocol.
- Seek assurance that the person remains in the best place for their care whilst awaiting bedded care daily from clinical leads and that these people have been escalated to named leads as per local protocol.
- Seek assurance that appropriate protocols for CYP with a learning disability and autistic children are being followed
ICB/ICP Actions
- Source a local bed or out of area placement (OAP) if no local bed available, with a view to repatriation of the person as soon as possible.
- Ensure protocols for CYP with a learning disability and autistic children are followed (e.g. known Dynamic Support Register and Care (Education) and Treatment Review)
- Take a leading role in sourcing complex social care placements working across a health and care footprint.
- Support discussions with Provider Collaboratives where required
- Seek assurance through escalation, that the person remains in the best place for their care whilst awaiting bedded care daily from clinical leads and escalate as per local protocol.
- Escalate disputes to regions to support resolution where all local escalations have been exhausted.
Actions for Acute Trust (working in partnership with the person and their care partner)
- Suitable member of staff to always remain with person awaiting admission to a MH bed; unless agreed that this is neither necessary nor appropriate, in which case a clear alternative plan should be in place.
- Ensure a timely referral is made to PLT in the first instance to support an MH assessment.
- A timely referral should be made to the Provider Collaborative, with all the necessary information, and ongoing communications with the Provider Collaborative should continue until a bed is sourced.
- For CYP with a learning disability, autism or SEND
- Ensure policy protocols or CYP with a learning disability and autistic children are followed – Dynamic Support Register and Care (Education) and Treatment Review
- Seek support from the learning disability liaison nurse and ensure reasonable adjustments and preferred communication methods are followed in line with Health Action and Behaviour Support plans.
- Ensure the person is known to the Community Intensive Support Team
- If the person cannot be rapidly transferred to a MH Trust, they should be cared for in the MH suite (if one is available) until they are admitted.
- If an appropriate bed is not located in a local MH Trust or an OAP within 12 hours of a decision to admit, they should be escalated to named leads within the Trust, with a clear timeline of expected actions and responsibilities. Medical/Nursing Director and the MH Medical Director should ensure that this is managed jointly, with daily conversations balancing the risk of the person staying in ED with the risks of them being in a paediatric bed.
- Consider early admission to an adolescent unit, paediatric ward whilst awaiting Tier 4 placement or complex social care placement.
- Ensure that an in-person review (or more frequent if appropriate) is carried out by a Consultant Psychiatrist to ensure appropriate management and to assess if admission is still required or if the person can be discharged or managed at home or in the community.
- Confirm with the person or their family/carer if community in reach/home treatment teams are involved in care planning and that social care arrangements are still in place.
- Discuss and agree the person’s treatment and movement/location with them and their care partner.
- No reduction in clinical priority for a MH bed should be attributed to the case due to any admission to a medical/community ward bedded area.
Actions for Mental Health Trust (working in partnership with the person and their care partner)
- The MH team should commence treatment and discharge planning as soon as possible, even if the person is still awaiting a bed.
- Confirm that community in reach/home treatment teams are involved in care planning where appropriate.
- If required, the MH team should seek an appropriate bed immediately. If none are available, or a long waiting list for beds is apparent, an OAP should be sought, but the Trust should only look for an OAP if no local beds are available and once other options have been exhausted.
- Rapid handover from the Acute to MH Trust should be facilitated where there is a safe environment in the MH Trust to do so.
- For CYP with a learning disability, autism or SEND
- Ensure policy protocols or CYP with a learning disability and autistic children are followed – Dynamic Support Register and Care (Education) and Treatment Review
- Seek support from the learning disability liaison nurse and ensure reasonable adjustments and preferred communication methods are followed in line with Health Action and Behaviour Support plans.
- Ensure the person is known to the Community Intensive Support Team
- Conduct an in-person review for all patients awaiting a mental health bed or review in the acute or community trust (or more frequent if appropriate) by a Consultant Psychiatrist to ensure appropriate management and to assess if admission is still required or if the person can be discharged or managed at home or in the community.
- If an appropriate bed is not located in a local MH Trust or an OAP within 12 hours of a decision to admit, they should be escalated within the Trust with a clear timeline of expected actions and responsibilities. Medical/Nursing Director and the MH Medical Director should ensure that this is managed jointly, with daily conversations balancing the risk of the person staying in ED with the risks of them being in a paediatric bed.
- No reduction in clinical priority for a MH bed should be attributed to the case due to any admission to a medical/community ward bedded area.
Older Adult Mental Health (Dementia)
Regional Actions
- Support conversations between ICBs and local authorities in sourcing complex combined health and social care placements where there’s a delay in transfer of care, risking a long wait in ED. Escalate to national team as per protocol.
- Seek assurance that the person remains in the best place for their care whilst awaiting bedded care daily from clinical leads and that these people have been escalated to named leads as per local protocol.
ICB/ICP Actions
- If no local bed available, source an out of area placement (OAP) with a view to repatriation of the person as soon as possible, depending on local OAP policies.
- Take a leading role in negotiating/sourcing complex social care placements working across a health and care footprint.
- Consider early admission to a community bed to improve the environment and allow de-escalation of the person’s confusion whilst awaiting dementia placement.
- Seek assurance that the person remains in the best place for their care whilst awaiting bedded care daily from clinical leads and escalate as per local protocol.
- Escalate disputes to regions to support resolution where all local escalations have been exhausted.
Actions for Acute Trust (working in partnership with the person and their care partner)
- Suitable member of staff to always remain with person awaiting admission to a MH bed; unless agreed that this is neither necessary nor appropriate, in which case a clear alternative plan should be in place.
- Ensure a timely referral is made to PLT in the first instance to support an MH assessment
- Person in ED is assessed by the MH team / PLT and where required, a bed for inpatient admission requested.
- Rapid handover of person to the MH team should be facilitated if the MH Trust has an appropriate area to manage them.
- If the person cannot be rapidly transferred to a MH Trust, they should be cared for in the MH suite (if one is available) until they are admitted.
- If an appropriate bed is not located in a local MH Trust or an OAP within 12 hours of a decision to admit, they should be escalated within the Trust with a clear timeline of expected actions and responsibilities. Medical/Nursing Director and the MH Medical Director should ensure that this is managed jointly, with daily conversations balancing the risk of the person staying in ED with the risks of them being in a G&A bed.
- Once admission is indicated, and if no rapid handover is available, the acute trust should refer to the Care Transfer Hub for a MH bed, if that is how MH beds are locally managed. Consider early admission to a community bed to improve the environment and allow de-escalation of the person’s confusion whilst awaiting dementia placement.
- Ensure that an in-person review (or more frequent if appropriate) is carried out by a Consultant Psychiatrist to ensure appropriate management and to assess if admission is still required or if the person can be discharged or managed at home or in the community.
- Confirm with the person or their family/carer if community in reach/home treatment teams are involved in care planning.
- Discuss and agree the person’s treatment and movement/location with them and their care partner, in line with local OAP policies and potential impact of multiple moves on the person’s condition.
- No reduction in clinical priority for a MH bed should be attributed to the case due to any admission to a medical/community ward bedded area.
Actions for Mental Health Trust (working in partnership with the person and their care partner)
- The MH team should get treatment and discharge planning started as soon as possible whilst the person is still awaiting a bed.
- Confirm that community in reach/home treatment teams are involved in care planning where appropriate.
- If required, the MH team should seek an appropriate bed immediately. If none are available, or a long waiting list for beds is apparent, an OAP should be sought, but the Trust should only look for an OAP if no local beds are available and once other options have been exhausted.
- Rapid handover from the Acute to MH Trust should be facilitated where there is a safe environment in the MH Trust to do so.
- Conduct an in-person review for all patients awaiting a mental health bed or review in the acute or community trust (or more frequent if appropriate) by a Consultant Psychiatrist to ensure appropriate management and to assess if admission is still required or if the person can be discharged or managed at home or in the community.
- Review inpatients daily to see if anyone could be discharged into the care of community teams to create capacity within local MH beds and dementia/functional wards.
- If an appropriate bed is not located in a local MH Trust or an OAP within 24 hours of a decision to admit, they should be escalated within the Trust with a clear timeline of expected actions and responsibilities. Medical/Nursing Director and the MH Medical Director should ensure that this is managed jointly, with daily conversations balancing the risk of the person staying in ED with the risks of them being in a G&A bed and in consideration of the Mental Health Act.
- No reduction in clinical priority for a MH bed should be attributed to the case due to any admission to a medical/community ward bedded area.
Complex Learning Disability and Autism/Social Care
Regional Actions
- Take a leading role in supporting conversations between ICBs and local authorities in sourcing complex combined health & social care placements where there’s a delay in transfer of care, risking a long wait in ED.
- Seek assurance that the person remains in the best place for their care whilst awaiting bedded care daily from clinical leads and escalate as per local protocol.
- Seek assurance appropriate steps being taken to comply with policy requirements (Dynamic Support Register and Care (Education) and Treatment Review)
ICB/ICP Actions
- Source a local bed or OAP if nothing local available after mutual aid sought, with a view to repatriation of the person as soon as possible.
- Take a leading role in sourcing complex social care placements working across a health and care footprint.
- Support discussions with Provider Collaboratives where required.
- Consider early admission to a community bed to improve the environment whilst awaiting complex social care placement.
- Ensure protocols for CYP with a learning disability and autistic children are followed (e.g. known Dynamic Support Register and Care (Education) and Treatment Review)
- Seek assurance that the person remains in the best place for their care whilst awaiting bedded care daily from clinical leads and escalate as per local protocol.
- Escalate disputes to regions to support resolution where all local escalations have been exhausted.
Actions for Acute Trust (working in partnership with the person and their care partner)
- Suitable member of staff to always remain with person awaiting admission to a MH bed; unless agreed that this is neither necessary nor appropriate, in which case a clear alternative plan should be in place.
- Ensure a timely referral is made to PLT in the first instance to support an MH assessment.
- For CYP with a learning disability, autism or SEND
- Ensure policy protocols or CYP with a learning disability and autistic children are followed – Dynamic Support Register and Care (Education) and Treatment Review
- Seek support from the learning disability liaison nurse and ensure reasonable adjustments and preferred communication methods are followed in line with Health Action and Behaviour Support plans.
- Ensure the person is known to the Community Intensive Support Team
- Person in ED is assessed by the MH team and, where required, a bed for inpatient admission OR a social care bed requested.
- If required, a timely referral should be made to the Provider Collaborative, with all the necessary information, and ongoing communications with the Provider Collaborative should continue until a bed is sourced.
- Rapid handover of the person to the MH or social care team should be facilitated if possible.
- If the person cannot be rapidly transferred to a MH Trust or a social care bed, they should be cared for in the MH suite (if one is available) until they are admitted.
- If an appropriate bed is not located within 12 hours of a decision to admit/transfer to social care, they should be escalated within the Trust with a clear timeline of expected actions and responsibilities. Medical/Nursing Director and the MH Medical Director should ensure that this is managed jointly, with daily conversations balancing the risk of the person staying in ED with the risks of them being in a G&A bed.
- Once admission is indicated, and if no rapid handover is available, the acute trust should refer to the Care Transfer Hub for a MH bed, if that is how MH beds are locally managed. Consider early admission to a community bed to improve the environment and allow de-escalation of the person.
- Ensure that an in-person review (or more frequent if appropriate) is carried out by a Consultant Psychiatrist/LDA Specialist to ensure appropriate management and to assess if admission is still required or if the person can be discharged or managed at home or in the community.
- Confirm with the person or their family/carer if community in reach/home treatment teams are involved in care planning and that social care arrangements are still in place.
- Discuss and agree the person’s treatment and movement/location with them and their care partner.
- No reduction in clinical priority for a MH bed should be attributed to the case due to any admission to a medical/community ward bedded area.
Actions for Mental Health Trust (working in partnership with the person and their care partner)
- The MH team should get treatment and discharge planning started as soon as possible whilst the person is still awaiting a bed.
- Confirm that community in reach/home treatment teams are involved in care planning where appropriate.
- For CYP with a learning disability, autism or SEND
- Ensure policy protocols or CYP with a learning disability and autistic children are followed – Dynamic Support Register and Care (Education) and Treatment Review
- Seek support from the learning disability liaison nurse and ensure reasonable adjustments and preferred communication methods are followed in line with Health Action and Behaviour Support plans.
- Ensure the person is known to the Community Intensive Support Team
- If required, the MH team should seek an appropriate bed immediately. If none are available, or a long waiting list for beds is apparent, an OAP should be sought, but the Trust should only look for an OAP if no local beds are available and once other options have been exhausted.
- Rapid handover from the Acute to MH Trust should be facilitated where there is a safe environment in the MH Trust to do so.
- Conduct an in-person review for all patients awaiting a mental health bed or review in the acute or community trust (or more frequent if appropriate) by a Consultant Psychiatrist/LDA Specialist to ensure appropriate management and to assess if admission is still required or if the person can be discharged or managed at home or in the community.
- If an appropriate bed is not located in a local MH Trust or an OAP within 12 hours of a decision to admit, they should be escalated within the Trust with a clear timeline of expected actions and responsibilities. Medical/Nursing Director and the MH Medical Director should ensure that this is managed jointly, with daily conversations balancing the risk of the person staying in ED with the risks of them being in a G&A bed.
- No reduction in clinical priority for a MH bed should be attributed to the case due to any admission to a medical/community ward bedded area.
8-65 years Mental Health
Regional Actions
- Take a leading role in supporting conversations between ICBs and local authorities in sourcing complex combined health & social care placements where there’s a delay in transfer of care, risking a long wait in ED.
- Seek assurance that the person remains in the best place for their care whilst awaiting bedded care daily from clinical leads and escalate as per local protocol.
- Seek assurance appropriate steps being taken to comply with policy requirements (Dynamic Support Register and Care (Education) and Treatment Review)
ICB/ICP Actions
- If no local bed available, source an out of area placement (OAP) with a view to repatriation of the person as soon as possible, depending on local OAP policies.
- Take a leading role in sourcing complex social care/housing placements working across a health and care footprint to decompress the local MH Trust.
- Ensure protocols for people with a learning disability and autism are followed (e.g. known Dynamic Support Register and Care (Education) and Treatment Review)
- Seek assurance that the person remains in the best place for their care whilst awaiting bedded care daily from clinical leads and escalate as per local protocol.
- Ensure MH crisis alternatives are in place with sufficient staffing and capacity, that these are listed on the DoS and that these are being promoted and activity within services monitored.
- Escalate disputes to regions to support resolution where all local escalations have been exhausted.
Actions for Acute Trust (working in partnership with the person and their care partner)
- Suitable member of staff to always remain with person awaiting admission to a MH bed; unless agreed that this is neither necessary nor appropriate, in which case a clear alternative plan should be in place.
- Ensure a timely referral is made to PLT in the first instance to support an MH assessment.
- Person in ED is assessed by the MH team and, where required, a bed for inpatient admission requested. Rapid handover of the person to the MH team should be facilitated if the MH Trust has appropriate area to manage them.
- If the person cannot be rapidly transferred to a MH Trust, they should be cared for in the MH suite (if one is available) until they are admitted.
- If an appropriate bed is not located in a local MH Trust or an OAP within 12 hours of a decision to admit, they should be escalated within the Trust with a clear timeline of expected actions and responsibilities. Medical/Nursing Director and the MH Medical Director should ensure that this is managed jointly, with daily conversations balancing the risk of the person staying in ED with the risks of them being in a G&A bed.
- Once admission is indicated, and if no rapid handover is available, the team should speak to the Care Transfer Hub about MH bed availability locally. The person should be added to the MH admissions list and if unlikely that a local bed can be found in a timely way, the system should start looking for an OAP.
- For autistic people and those with a learning disability, ensure policy protocols and health action plans are followed and make any reasonable adjustments as required, ensure they are known to the Community Intensive Support Team.
- Ensure that an in-person review (or more frequent if appropriate) is carried out by a Consultant Psychiatrist to ensure appropriate management and to assess if admission is still required or if the person can be discharged or managed at home or in the community.
- Confirm with the person or their family/carer if community in reach/home treatment teams are involved in care planning.
- Discuss and agree the person’s treatment and movement/location with them and their care partner in line with local OAP policies and potential impact of multiple moves on the person’s condition.
- No reduction in clinical priority for a MH bed should be attributed to the case due to any admission to a medical/community ward bedded area.
Actions for Mental Health Trust (working in partnership with the person and their care partner)
- The MH team should get treatment and discharge planning started as soon as possible whilst the person is still awaiting a bed.
- Confirm that community in reach/home treatment teams are involved in care planning.
- If required, the MH team should seek an appropriate bed immediately. If none are available, or a long waiting list for beds is apparent, an OAP should be sought, but the Trust should only look for an OAP if no local beds are available and once other options have been exhausted.
- Rapid handover from the Acute to MH Trust should be facilitated where there is a safe environment in the MH Trust to do so.
- Conduct an in-person review for all patients awaiting a mental health bed or review in the acute or community trust (or more frequent if appropriate) by a Consultant Psychiatrist to ensure appropriate management and to assess if admission is still required or if the person can be discharged or managed at home or in the community.
- If an appropriate bed is not located in a local MH Trust or an OAP within 12 hours of a decision to admit, they should be escalated within the Trust with a clear timeline of expected actions and responsibilities. Medical/Nursing Director and the MH Medical Director should ensure that this is managed jointly, with daily conversations balancing the risk of the person staying in ED with the risks of them being in a G&A bed.
- For autistic people and those with a learning disability, ensure policy protocols and health action plans are followed and make any reasonable adjustments as required.
- No reduction in clinical priority for a MH bed should be attributed to the case due to any admission to a medical/community ward bedded area.
Chair’s Report from the Quality Committee meeting on 11 September 2025
- Paper title: Chair’s Report from the Quality Committee meeting on 11 September 2025
- Date of meeting: 25 September 2025
- Presented by: Dr Frances Healey, Non-executive Director and Chair of the Quality Committee
- Prepared by: Kerry McMann, Head of Corporate Governance
This paper supports the Trust’s strategic objective/s (SO):
- SO1 – We deliver care that is high quality and improves lives.
- SO3 – We use our resources to deliver effective and sustainable services.
This paper relates to the Trust’s strategic risk/s
- SR1 – Quality including safety assurance processes
- SR2 – Delivery of the Quality Strategic Plan
Committee details:
- Name of Committee: Quality Committee
- Date of Committee: 11 September 2025
- Chaired by: Dr Frances Healey, Non-executive Director
Alert – items to alert the Board to:
- No items to alert the Board to.
Advise – items to advise the Board on
- The committee supported a proposal to extend the term of the Trust’s Research Strategy from three years to five years.
Assure – items to provide assurance to the Board on
- The committee reviewed the BAF, paying particular attention to SR1 and SR2. It was assured that SR1 and SR2 were being adequately controlled.
- The committee considered the Trust’s position against its 2025/26 organisational priorities relevant to quality at the end of quarter one and was assured as to the systems and processes in place for monitoring and supporting the delivery of each priority’s high-level milestones and underpinning tasks.
- The committee received the Medicines Optimisation Group (MOG) Annual Report for 2024/25 and agreed that the Medicines Optimisation Group was fulfilling its Terms of Reference. It noted the challenges that had been faced by the Pharmacy Service during the year relating to vacancies and business continuity but was reassured on the progress that had been made against the recovery plan. The committee discussed its role in relation to medicines and an action was agreed for Dr Hosker and Mrs Edwards to ensure future reports provide sufficient assurance on medicines safety and effectiveness.
- The committee received a report which provided data on reported falls in the Trust between April 2024 and March 2025. It was pleased to hear that there had been a 13% reduction in reported falls in 2024/25 compared to 2023/24 and acknowledged the progress that had been made in this area since the committee last received an update in September 2024. The committee was assured that falls reported in the Trust were being considered in a robust and governed way and that data was being used to drive improvement work.
- The committee received a report which outlined the improvement work that had been undertaken to change the Trust’s approach to enhanced care and observations and to engage with the national Enhanced Therapeutic Observations and Care (ETOC) Programme.
- The committee received a report which provided information on the arrangements to ensure patient safety in clinical trials. It also discussed the scope of research reporting to the Quality Committee
- The committee received a report which provided an update on the work undertaken to change the Trust’s approach to clinical risk assessment. It recognised the success of the roll out of the Risk Assessment and Safety Planning (RAMP) tool and acknowledged the key factors in the successful rollout, which included clear identification of subject matter experts, decision-making authority for service representatives and dedicated project leadership.
- The committee received a supplementary report which provided an overview of mortality data for quarter three of 2024/25, which was mistakenly omitted from the previous Learning from Deaths Report that was presented to the committee in June 2025.
- The committee reviewed presentations which provided the highlights of the Rehabilitation Service’s and the Gender Identity Service’s Annual Quality Report, focusing on how the services had scored themselves against the STEEEP dimensions. The committee was pleased to hear that the Rehabilitation Service had received a Royal College of Psychiatry Rehabilitation Network Award. It noted that work was ongoing to improve productivity within the Gender Identity Service using tools such as artificial intelligence and heard about plans for an AI-focused strategic session and plans to use video case studies to disseminate learning. Overall, the committee was assured that the services had good systems in place for understanding their quality issues and to drive improvements, and good knowledge of their strengths and weaknesses in relation to learning, culture and leadership. The committee was also assured that the Executive Team had a clear understanding of the services’ strengths, weaknesses, challenges and blind spots and how issues were being managed.
- The committee received the Combined Quality and Workforce Performance Report and reviewed the data provided, acknowledging that workforce data continued to be discussed at Workforce Committee and at Board. The committee also acknowledged that the System Oversight Framework had been replaced by the NHS Oversight Framework and that work was ongoing to update reports to ensure the correct data was being reported.
- The committee received a report which described the outcomes from a review of NHS England’s Patient Safety Healthcare Inequalities Reduction Framework (PSHIRF) against the Trust’s Improving Health Equity Strategic Plan 2025-29 to ensure the Trust’s plan aligned with the PSHIRF. It was assured that the PSHIRF guiding principles and further opportunities for local delivery were captured within existing programme delivery plans.
- The Committee received a report on Medical Devices and was assured on the governance, monitoring, and management of medical devices in the Trust. It was agreed that this would be an annual report.
- The committee acknowledged that an opinion of significant assurance had been given in relation to an internal audit on the systems and processes for monitoring Patient Safety Incident Response Framework (PSIRF) compliance and escalation at the Trust.
Refer – Items to be referred to other Committees:
- No items to refer to other committees.
Recommendation
The Board of Directors is asked to note the update provided.
Cover sheet for the Specialist Supported Living Service Quality and Oversight Paper
- Paper title: Specialist Supported Living Service Quality and Oversight Paper
- Date of meeting: 25 September 2025
- Presented by: Nichola Sanderson, Executive Director of Nursing
- Prepared by: Alison Quarry, Deputy Director of Nursing
This paper supports the Trust’s strategic objective/s (SO):
- SO1 – We deliver great care that is high quality and improves lives
This paper relates to the Trust’s strategic risks (SR):
- SR1 – Quality including safety assurance processes
- SR7 – Plan and deliver services that meet the health needs of the population we serve.
Executive summary
This report provides an overview of the key standards and quality of care including the governance and oversight of Specialist Supported Living Service (SSLS). It aims to highlight this through the Quality Peer Review process which was carried out reflecting the CQCs fundamental standards of care and other significant workstreams.
Do the recommendations in this paper have any impact upon the requirements of the protected groups identified by the Equality Act? No
Recommendation
The Board is asked to be assured of the work being undertaken to deliver the SSLS and to manage the recruitment challenges outlined in this report.
Overview of the governance and standards of care in relation to Specialist Supported Living Service
INTRODUCTION
This report provides an overview of the key standards and quality of care including the governance and oversight of Specialist Supported Living Service (SSLS). It aims to highlight this through the Quality Peer Review process which was carried out reflecting the CQCs fundamental standards of care and other significant workstreams.
The Specialised Supported Living Service (SSLS) provides accommodation to individuals with learning disabilities and complex health needs at 16 locations across Leeds. The service is predominantly staffed with Support Workers (Band 3) or Senior Support Workers (Band 4). The service is funded by Adult Social Care for 250 WTE; 90% of this workforce is made up of either Senior or Support Workers, the remaining 10% being either Band 6 or 7 staff (registered and non-registered) who are responsible for operational and clinical leadership in the service.
Service User Involvement
Service User Involvement is fundamental to the SSLS. The service uses multiple methods and approaches to ensure this remains central to everything they do.
The service holds an annual Have Your Say event which offers various approaches to providing feedback. A detailed report is generated following these events and shared across the governance structures to inform service improvement and to ensure learning and reflection on feedback. The most recent ‘Your Say’ event took place in August 2025. The corresponding report will be available for distribution shortly. The involvement of individuals with lived experience is integral to the Learning Disability Clinical Governance Forum and plays a vital role in both shaping and enhancing the development of the service. Resident feedback from SSL is regularly reviewed during the Learning Disability Clinical Governance Meeting to assess and consider any learning and improvement.
A fantastic example of how this adds value to the service can be demonstrated through September’s Clinical Governance Forum whereby one of the SSLS residents attended, accompanied by their primary support worker, to share their lived experience at SSL and to contribute to discussions around the Person-Centred Review (PCR) process.
The PCR process is a facilitated meeting that puts the individual and their family at the centre of the review process to develop person-centred outcomes for their support plan. The process involves gathering information about what is important to the individual, their strengths, and their future aspirations. The intention is to identify what is working well but also what is not working well and offers the opportunity to showcase the resident’s accomplishments over the past 12 months while developing their objectives for the forthcoming year. A collection of photographs and documented experiences were used at the governance forum to facilitate the acknowledgement and celebration of these achievements.
These discussions then lead to jointly agreed, person-centred outcomes, which in turn creates more effective care to meet the individual’s needs.
Quality Peer Review for Specialised Living Support Services
The Trusts Quality Peer Review process aims to improve care for the people who use our services by ensuring they are as safe as possible. Using the Care Quality Commissions Quality Statements (previously Key Lines of Enquiries), a team of peer reviewers visit services across the Trust to review the quality of care being delivered. The Quality Peer Reviews provide teams with an opportunity to share good practice and consider the challenges of care delivery through highlighting areas for improvement.
A Quality Peer Review was carried out within Specialised Living Support Services, with visits to two of our houses, Methley Lodge and Pudsey Bungalow. The review was led by the Head of Clinical Governance and Quality and included staff from the Safeguarding Team, Mental Health Legislation Team, and Professional Leads (Allied Health Professional and Nursing).
As part of the Quality Peer Review the reviewing team carried out the following:
- observed the living environments
- reviewed the quality of documentation
- reviewed capacity assessments
- observed interactions with staff, tenants, and their families
- reviewed learning from incidents and governance arrangements.
The Quality Peer review demonstrated evidence of high-quality care being delivered and highlighted areas of good practice. The environment was welcoming with tenants encouraged to decorate their own bedrooms and clearly evidencing a feeling of ‘home’. An agreement leaflet for tenants which helped describe risk and safety in relation to what was required to help tenants feel safe in the home was developed for all residents.
All tenants had support plans in place that had been coproduced and detailed triggers which may escalate their presentation. Staff clearly knew residents well and had a good understanding of their plans of care. Staff demonstrated their approach to working alongside tenants to deescalate situations using least restrictive practice guided by the plans of care.
At the time of the review vacancies across the service had improved with staff and tenants describing that staffing levels made them feel safe.
Feedback from carers was overwhelmingly positive with carers reporting; “staff treated (her daughter) with kindness, dignity and respect”. Carers also reported they felt updated and informed about their relative’s care and treatment.
The findings from the Quality Peer Review were shared with the service and through their governance forums. No patient safety concerns were identified during the visit and therefore it was agreed that no further reviews were required outside of the annual cycle and schedule.
Quality and performance Indicators
The chart below outlines quality and performance across the SSLS which includes compliance data relating to Clinical Supervision, Appraisals, and Mandatory Training for the past six months.
Clinical Supervision has achieved 100% compliance across the data period, with the exception of April 2025. Compliance levels were lower at one of the SSL houses, primarily due to various forms of leave. This had a subsequent impact on the overall compliance figures for the service.
Compliance rates for both Appraisals and Mandatory Training have remained around 80% across the same period.

Patient Safety Incidents
The number of patient safety incidents recorded over the past six months, highlighting a reduction in incidents during August 2025 which is demonstrated in the table below.

A targeted initiative focusing on medication safety has recently been introduced, which is suggested to have contributed to a sustained decline in medication-related incidents.
The Professional Lead Nurse delivered medication awareness training to senior leaders within the service, who subsequently cascaded the training to the remaining staff. The training package incorporated key learning points identified through the review of recent medication-related incidents. In addition, the service has been supported to develop comprehensive guidance and a competency framework to clearly define skills and knowledge to enable staff development, enhance learning, and provide assurance regarding patient safety. The framework has been rolled out across the SSLS and the effectiveness will be evaluated.
The table below demonstrated the total number of patient safety incidents associated with medication errors reported over the most recent six-month period, compared with the corresponding timeframe in the previous year. In the six months of 2024, a total of 32 incidents were recorded which predated the workstream to improve medication awareness and associated training. This figure decreased to 22 during the same period in 2025 following the training, indicating an overall reduction in reported cases
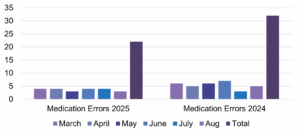
Recruitment
As demonstrated through September’s Safer Staffing Board the highest number of vacancies for Health Support Workers are situated within the Specialised Supported Living Service with 53 WTE vacancies across the service. Ongoing recruitment initiatives are currently in progress aimed at addressing existing workforce gaps. The service is particularly engaged with the apprenticeship agenda and have a high volume of Apprentice Health Support Workers in post. The service has a robust assessment centre recruitment process in place which involves service users keeping in live with service users being central to their approach.
The Safer Staffing Forum approved a new proposal in September which set out an innovative approach to recruitment which addresses the current challenges being faced as described across our care services. The recruitment campaign will target those areas with the highest number of vacancies and is set to use a variety of methods including the Leeds Health and Care Academy (LHCA) Talent Hub reverse recruitment programme. The Talent Hub can screen applicants’ visa status and apprenticeship eligibility in addition to checking role suitability before putting forward candidates for interview. The roles will be via the LHCA Talent Hub website and shared with city-wide employability partners. A significant social media campaign will accompany the approach.
Summary
The SSLS has demonstrated through this report that high quality care is being delivered across the service which is evidenced through the Quality Peer Review process. The service holds lived experience at the centre of its approach which is integral to all aspects of care deliver and governance. Where improvement initiatives are identified, workstreams are developed to address which has been demonstrated through this report evidencing where this can add value and improve patient safety.
There does remain recruitment challenges within the service which are discussed through the Safer Staffing Forum with plans in place to improve this position through an innovative proposal.
Various recruitment initiatives continue to be coordinated within the service including Apprentice Support Worker recruitment.
The Board is asked to be assured of the work being undertaken to deliver the SSLS and to manage the recruitment challenges outlined in this report.
Alison Quarry
Deputy Director of Nursing
September 2025
Contributions from members of the Nursing and Professions Team
Cover sheet for the LYPFT 2-Month Safer Staffing Review Report
- Paper title: LYPFT 2-Month Safer Staffing Review Report
- Date of meeting: 25 September 2025
- Presented by: Nichola Sanderson, Director of Nursing
- Prepared by: Alison Quarry, Deputy Director of Nursing; Miriam Blackburn, Head of Nursing; Jennifer Connelly, Professional Lead Nurse; and Adele Sowden, E-Rostering Team Manager
This paper supports the Trust’s strategic objective/s (SO):
- SO1 – We deliver great care that is high quality and improves lives
- SO2 – We provide a rewarding and supportive place to work
- SO3 – We use our resources to deliver effective and sustainable services
This paper relates to the Trust’s strategic risks (SR):
- SR1 – Quality including safety assurance processes
- SR3 – Culture and environment for the wellbeing of staff
Executive summary
This paper draws on the NHS National Quality Board (2016) reporting requirements to ensure that nursing and care staffing, capacity and capability is enabled to deliver high quality care and the best possible outcomes for patients whilst balancing quality and financial objectives and acknowledging the ongoing pressures experienced in relation to staffing and resource.
The paper contains a high-level overview of data and analysis to provide the Board of Directors and the public with information on the position of Leeds and York Partnership Trust wards staffing against safer staffing levels between 1st April to 31st May 2025 including unify data for March 2025.
This report details that 1 clinical shift during that period did not have a registered nurse and outlines the mitigations in place to ensure patient safety.
The paper draws focus to 4 clinical areas where there is either significant Registered Nurse and Health Support Worker vacancies or are using significantly higher numbers of staff above the planned establishment and provides data to demonstrate the impact through a series of quality indicators outlining any mitigation or workstreams to support the current workforce challenges. Not include embedded items anywhere in the cover sheet.
Do the recommendations in this paper have any impact upon the requirements of the protected groups identified by the Equality Act? No
Recommendation
The Board is asked to:
- Note the content of the report.
- Be assured that arrangements are in place to monitor, support and mitigate any impact of reduced staffing levels or skill mix in relation to patient safety.
Safer Staffing: Inpatient Services – June and July 2025
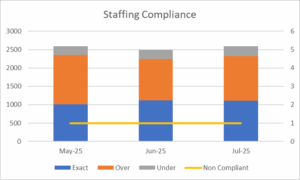
| Number of Shifts | |||
| May | June | July | |
| Exact | 1009 | 1114 | 1112 |
| Over Compliance | 1341 | 1134 | 1204 |
| Under Compliance | 241 | 249 | 273 |
| Non-Compliant | 1 | 1 | 1 |
Risks: Registered Nursing vacancies continue to be a major theme across the focussed areas highlighted by the Unify data (Appendix A).
Mitigating Factors: Reduced RN fill rates are being partially mitigated in many of our units by increasing Healthcare Support Worker (HSW) duties through Bank and Agency staffing to reach minimum staffing numbers. The use of a multi-professional approach to support establishments through using the workforce flexibly and effectively to deliver patient care continues to be progressed.
Narrative on Data Extracts Regarding LYPFT Staffing Levels on x28 Wards during June and July 2025: This is the whole time equivalent (WTE) number of staffing posts the inpatient wards are funded for to deliver planned level of care and interventions within their speciality by shift.
Staffing compliance: This tells us whether the wards met the planned numbers of staffing during a shift. The planned staffing numbers do not necessarily reflect the actual staffing need on any given duty as this may fluctuate dependent on current patient group and need.
Exact or Over Compliant shifts: The compliance data demonstrated an increase in the number of shifts which were staffed exactly as planned in June and July 2025. There was a decrease in the number staffed above the planned establishment of Registered Nurse and Health Support Worker duties during the month of June and July 2025. The largest proportion of clinical shifts are working over the planned establishment. This is predominantly in response to an increase in enhanced care and the use of observation and engagement to deliver safe and effective care.
The staffing escalation and deployment protocol which was developed as part of the staffing escalation workstream is currently being embedded in practice across inpatient areas. The protocol will provide assurance that the correct steps for escalation of staffing shortfalls has occurred to support timely resolution, which in turn is anticipated to reduce reliance on temporary staffing. The work carried out aimed to understand developed cultures around different professions and roles on our inpatient wards. The group considered the cultural shift required to support and facilitate inpatient teams to use their workforce flexibly and effectively, in line with the Trust staff escalation protocol.
*(Note this differs from the unify report in Appendix A which shows the total hours over the month rather than on a shift-by-shift basis).
Non-Compliant Shifts: This metric represents the number of shifts where no Registered Nurses were on duty. There have been two shifts during the reporting period where there has been no Registered Nurse on duty. On the 11 June at 3 Woodland Square, due to sickness there was no Registered Nurse for the early shift. The band 4 Nursing Associate took responsibility for the administration of medication with oversight from the Registered Nurse working at 2 Woodland Square.
The night shift on the 19 July at Red Kite View, PICU was covered with a Registered Nurse and Nursing Associate, the Registered Nurse was injured on duty and had to leave the ward at 10pm. The Registered Nurse from the adjoining ward at Red Kite View took charge of both wards supported by the Nursing Associate on duty. The Nursing Assoicate was responsible for the administration of medication which is within scope of practice.
Vacancies
Below indicates the total number of vacancies across each service as reported on ECHO in July 2025. This is across the multidisciplinary teams and not solely related to Registered Nurses and Health Support Workers, which are roles traditionally viewed in the safer staffing figures. Alongside this are the Registered Nurse and Band 3 Health Support Worker vacancies taken from the finance figures for July.
Although Registered Nurses and Health Support Workers are those reported in the safer staffing figures. It is important to recognise the range of roles within the multidisciplinary teams for providing safe and effective care in our ward establishments which is not accurately captured in the unify data (Appendix A). The highest number of vacancies are within the Older People’s Service, Acute Inpatient and PICU and the Specialised Supported Living Service.

Below indicates the total % of vacancies across each service as reported on ECHO in July 2025. This is across the multidisciplinary teams and not solely related to Registered Nurses and Health Support Workers, which are roles traditionally viewed in the safer staffing figures. The highest percentage of vacancies are within the York Forensic Service, Acute Inpatient and PICU and the Specialised Supported Living Service. Ongoing recruitment initiatives are currently in progress, aimed at addressing existing workforce gaps. These efforts are complemented by the scheduled onboarding of Registered Nurse Preceptees, who are set to commence employment in September and October 2025. Together, these measures are expected to contribute significantly to reducing the current vacancy levels across inpatient services.
The chart also includes the % vacancies for Registered Nurses and Band 3 Healthcare Support Workers for each service taken from the finance data for July 2025.

Safer Staffing Group
The Trusts Safer Staffing Steering Group continues to meet monthly with a focus on reviewing the safety and quality of staffing across inpatient services, progressing improvement workstreams in relation to staffing and overseeing the staffing establishment review process. This includes the oversight of 6-monthly MHOST data collection, with the next data collection due to take place throughout September 2025.
Over the next 12 months, LYPFT will be participating in a national programme focused on improving our approach to therapeutic observations and engagement within our inpatient services. Increased observations are the most frequently cited reason for additional staffing and wards working above the establishment. The work aims to implement a set of best-practice principles that recognise enhanced observations as inherently restrictive practice and potentially harmful, despite their safety intentions. This will result in a full review of our current procedure and training package. The project will report into the Positive and Safe Group and provide regular updates via the Safer Staffing Steering Group.
Summary
A reduction in overall vacancies for inpatient areas is predicted to continue to improve over the coming months following recruitment campaigns and preceptee nurses who will join inpatient areas. There has been the need for additional staffing above the planned establishment to deliver safe and effective care, particularly to support service users requiring enhanced observations. Staffing pressures are currently mitigated through the combination of temporary staffing and substantive staff working additional duties alongside more effective integration of our multi-disciplinary teams.
The delivery of care through the multidisciplinary team and the professional specific roles which is not captured in the planned staffing establishment should be considered when reviewing the data. Workstreams commissioned through the Safer Staffing Forum continue to progress which are focused on a cultural shift moving away from viewing inpatient staffing in the traditional roles of Nurses and Health Support Workers and toward an integrated MDT approach to focus on improving the quality of care delivered to our service users.
Recommendations:
The Board is asked to:
- Discuss and note the content of the report.
- Be assured of the arrangements in place to monitor, support and mitigate the impact of reduced staffing levels and skill mix in relation to quality and safety in inpatient setting
Appendix A
Safer Staffing: Inpatient Services June 25
Fill rate indicator return
Staffing: Nursing, Care Staff and AHPs

Safer Staffing: Inpatient Services July 25
Fill rate indicator return
Staffing: Nursing, Care Staff and AHPs
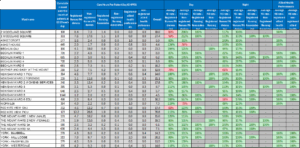
Cover sheet for the Safer Staffing Establishment Review
- Paper title: Safer Staffing Establishment Review
- Date of meeting: 25 September 2025
- Presented by: Nichola Sanderson, Executive Director of Nursing
- Prepared by: Alison Quarry, Deputy Director of Nursing; Miriam Blackburn, Head of Nursing; and Jennifer Connelly, Professional Lead Nurse.
This paper supports the Trust’s strategic objective/s (SO):
- SO3 – We use our resources to deliver effective and sustainable services
This paper relates to the Trust’s strategic risks (SR):
- SR1 – Quality including safety assurance processes
- SR3 – Plan and deliver services that meet the health needs of the population we serve
Executive summary
This paper sets out the process, findings and recommendations for Leeds and York Partnership Foundation Trust (LYPFT) 2024/2025 Annual Establishment Review.
The annual establishment review has been conducted in line with national regulatory requirements. Demonstrating sufficient staffing is one of the fundamental quality and safety standards required to comply with the Care Quality Commission (CQC) regulation. The purpose of this report is to inform the Trust Board of the findings from the annual establishment reviews and any subsequent recommendations relating to the planned establishments reviews in LYPFT inpatient areas to enable safe and effective care to be delivered.
The paper details the evidence based outcomes and recommendations across the 28 inpatient wards following the use of a triangulated approach which includes using an evidence-based tool (MHOST) and the use of professional judgement, clinical indicators and benchmarking data.
The paper describes that many wards were routinely utilising excess staffing above that of their agreed baseline establishments. It was acknowledged that this does not automatically lead to the need for an increase in establishment and in some clinical areas the review of clinical practice, skills and competencies were required before further consideration of any increase to staffing is recommended.
The recommendations have been made at a time when significant workstreams which are linked to the Trust’s 14 priorities are commencing, which will in turn impact on staffing and workforce. This was considered as part of the final recommendations and the anticipated outcomes of the workstreams were informed decision making.
The findings did however recommend that an uplift in establishment was agreed across the Acute Inpatient Service increasing safer staffing numbers by x 1 Band 3 practitioner per duty.
The paper has been tabled at the appropriate governance forums including Finance and Performance where the uplift has been agreed.
Do the recommendations in this paper have any impact upon the requirements of the protected groups identified by the Equality Act? No
Recommendation
The Board are asked to:
- Note and be assured by the content of the paper
- Support the recommendations as outlined in the paper
Safer Staffing Annual Establishment Review Paper
1.0 Introduction
Leeds and York Partnership Foundation Trust (LYPFT) annual establishment review has been conducted in line with national regulatory requirements. Demonstrating sufficient staffing is one of the fundamental quality and safety standards required to comply with the Care Quality Commission (CQC) regulation. The purpose of this report is to inform the Trust Board of the findings from the annual establishment reviews and any subsequent recommendations relating to the planned establishments reviews in LYPFT inpatient areas to enable safe and effective care to be delivered.
2.0 Background and Context
The establishment review process complies with the requirements set within the National Quality Board report (NQB 2016).The NQB document supports NHS providers to deliver the right staff, with the right skills in the right place, at the right time. It outlines the expectations for nursing and midwifery staffing through the use of a triangulated approach to staffing decisions based on patient’s needs, acuity, and risk, using evidence-based tools and the use of professional judgement.
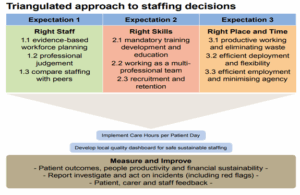
In January 2018, the NQB published an improvement resource that makes specific reference to how these expectations are adopted within mental health services. The guidance acknowledges that staffing reviews need to consider other inpatient roles that support nursing staff to provide good care; this has been considered in this review.
LYPFT have adopted use of the Mental Health Optimal Staffing Tool (MHOST) as its evidence based mental health workforce tool. The MHOST was created with the support of Health Education England. It has been developed alongside clinical leaders and workforce staff in Mental Health Trusts and rigorously assessed and validated.
3.0 Establishment Review Process
Prior to any establishment review taking place within the organisation, data collection from a range of sources is required. The process included data collection from a variety of sources which was reviewed and scrutinised at an establishment review outcome meeting attended by senior leaders from across the Trust. The process was applied to all wards across the organisation.
3.1 Purpose
Each review focused on identifying whether the current planned (budgeted) establishments across our inpatient wards remained appropriate to deliver safe and effective care through the application of the triangulated approach including the use of MHOST data, quality indicators and professional judgement.
3.2 Scope
LYPFT provides inpatient care across 28 Mental Health and Learning Disability Wards. Establishment reviews were carried out on all inpatient areas.
3.3 MHOST Use and Data Collection
The data collectors for each ward were either band 6 or 7 Registered Nurse’s (RNs) or Allied Health Professionals (AHP’s) and were kept to a minimum (2-3 colleagues) to ensure consistency. Each ward carried out inter-rater reliability.
The first MHOST data collection period was completed in September 2023 with a further data collection completed in March 2024; this provided the initial data to support evidence-based workforce planning. Two sets of data collection of 28 days are required as a minimum before the data should be considered as part of the staffing establishment planning.
3.4 Quality Indicator and Workforce Metrics
Examples of what can be considered as a quality indicator are listed within the NQB guidance. Services were asked to consider any quality indicators that may be particularly important to their service. This data was then taken from the Trusts ECHO system for the previous 12 months. This information was gathered by either Professional Lead Nurses or the individual service.
Examples of quality indicators include but were not limited to:
- Incidents including serious incidents
- Staff metrics including sickness, stress, or mental health related sickness
- Clinical supervision, appraisal, and compulsory training compliance
- Length of stay
- Complaints
- Service user feedback
In addition, benchmarking data was used. This included inpatient wards across LYPFT and also other mental health organisations inpatient areas of a similar function i.e. female acute inpatient.
The data described above was reviewed collectively and considered based on the professional judgement of those in the room throughout the meeting. Professional judgement can be described as the use of accumulated knowledge and experience in order to make an informed decision. A professional judgement framework was referred to in order to support discussions.
The outcome of the review of data and discussion led to recommendations for each clinical area.
4.0 Results
It was found that many wards were routinely utilising excess staffing above that of their agreed baseline establishments. It was acknowledged that this does not automatically lead to the need for an increase in establishment and in some clinical areas the review of clinical practice, skills and competencies were required before further consideration of any increase to staffing is recommended. The process and analysis via the MHOST tool suggests that additional staffing is however required in some areas based on the triangulated approach.
4.1 Summary of Key Points from Establishment Reviews
| Ward | Outcome | Actions |
| Asket Croft & House | Recommendation to increase staffing establishment at Asket Croft/ | Recommendations detailed below
Team to review the budget vs the roster template outside the meeting due to inconsistency. Asket House have spent a period of time working below the budgeted establishment with potential impact on staff experience and shift planning. It was agreed that Asket House should begin to ensure it was working to agreed establishment. |
| Becklin
Wards 1 & 5 |
Recommendation to increase staffing establishment | Recommendations detailed below 4.3 |
| Becklin
Wards 3 & 4, Newsam Ward 4 |
Recommendation to increase staffing establishment | Recommendations detailed below 4.3 |
| Crisis Assessment Unit (CAU). Budget/staffing establishment amalgamated with street triage and section 136. | Current Establishment Satisfactory
Unpredictability of activity in section 136 and street triage has created challenges when determining the staffing establishment. |
Data collection was completed when CAU was functioning as a female acute ward. Further MHOST data collection required on its return to its primary function as a 72-hour assessment unit. |
| Forensic Wards Leeds | Current Establishment Satisfactory | Skill mix review specifically around Band 3 role. |
| Forensic Wards York (provider collaborative) | Recommendation to increase staffing establishment in Riverfields ward | Recommendations detailed below 4,3
Bed occupancy low during period of MHOST data collection for other wards, further data collection scheduled during period of increased bed occupancy. |
| Mill Lodge | Current Establishment Satisfactory | Review in line with routine establishment review. |
| Mother and Baby Unit | Requires further data collection | Agreed to review establishment again following further MHOST data collection due not being representative typical occupancy and investment in extended unit. |
| National Inpatient Centre for Psychological Medicine (NICPM) | Current Establishment Satisfactory | There was a misalignment between the roster and budget. A meeting was subsequently required with the service operational managers, finance, and People Analytics to resolve. |
| PICU Newsam Centre | Current Establishment Satisfactory | Review provision of activity coordinator. |
| Red Kite View PICU | Recommendation due to review of clinical model a decision to pause this has been made and to be reviewed in 6 months. | Review of clinical model |
| Red Kite View GAU | Current staffing establishment satisfactory, requested adjusted skill mix. | Adjust skill mix – reduce Registered Nurse cover during the day by one and increase Health Support Workers by one. The ward has been working on reduced bed capacity during the data collection period and with significant nursing vacancies that have meant that they have been unable to meet the current funded establishment of four Registered Nurses per day shift. Therefore, it is felt that a planned reduction in Registered Nurses will not impact on the quality of care being delivered. |
| The Mount Ward 1 | Current Establishment Satisfactory | Clinical team to complete piece of work related to the use of observation and engagement in the environment in advance of next review. |
| The Mount Ward 2 | Recommendation to increase staffing establishment | Recommendations detailed below 4.3 |
| The Mount Wards 3 & 4 | Current Establishment Satisfactory | Complete skill mix review. |
| Ward 5 Newsam Centre | Current Establishment Satisfactory | The establishment is appropriate for the current position within the Newsam Centre; however, discussions included the need for uplift with the move to a stand-alone unit in 2025. Business case to be completed to reflect. |
| Woodlands 2 & 3 | Current Establishment Satisfactory | Skill mix review- explore benefits of introducing non-medical prescriber. |
| Yorkshire Centre for Eating Disorders (YCED) (provider collaborative) | Recommendation to increase staffing establishment | Recommendations detailed below 4.3 |
4.2 Areas with Recommendations to Increase LYPFTs Staffing Establishment
The evidence reviewed demonstrated that a small number of LYPFT’s inpatient wards are under resourced resulting in a reliance on increasing the safer staffing workforce each duty based on clinical need. Temporary workforce is predominantly used to fill these duties.
Local benchmarking data from across the ICS further reinforces that a small number of wards are under resourced when comparing wards of a similar function.
The staffing establishment review has enabled evidence-based recommendations to be made to increase the staffing establishment across the service in some clinical areas. However, the recommendations have been made at a time when significant workstreams which are linked to the Trust’s 14 priorities are commencing, which will in turn impact on staffing and workforce. It therefore would be impetuous to make significant workforce changes at this time to reflect the complete findings with the possibility that the impact of these initiatives may result in a different outcome.
All inpatient wards are engaged in the Enhanced Therapeutic Observations of Care (ETOC) Programme.
The programme is a national initiative addressing the rise in observation and engagement practices across inpatient wards, which are now recognised as restrictive practice. LYPFT wards show elevated staffing due to ETOC demands, especially in female acute wards.
The programme is expected to
- Standardise training and competencies for all staff, including temporary workers.
- Improve oversight, data collection, and reflective practice.
- Ensure registered professionals lead complex ETOC interventions.
- Reduce reliance on temporary staff by refining care delivery models.
The programme will support the Trust’s workforce efficiencies programme which forms one of the 14 priorities set by the Trust.
The acute care pathway which includes our acute inpatient wards are engaged in the Inpatient Quality Transformation Programme (IQTP) which forms one of the Trusts 14 priorities.
The overarching programme is led by NHS England to modernise Mental Health, Learning Disability, and Autism Inpatient care with the aims to improve patient flow, reduce out-of-area placements, and embed compassionate, person-centred care.
The programme informs a full review of the clinical model and workforce planning using six national principles (Valuing, Accessible, Humane, Equitable, Therapeutic, Collaborative).
It is anticipated that the outcomes of the two programmes together will reshape workforce design, reduce unnecessary staffing pressures, and enhance care quality. Progress will be monitored along with monitoring the use of temporary staffing to identify any reduction as a result of this.
4.3 Recommendations from the establishment review process
Key Findings of the Acute Inpatient Service
- Many wards are operating above their budgeted staffing levels, often relying on temporary staff.
- Several wards require increased staffing to meet clinical demands and improve care quality.
- Acute inpatient wards, particularly female wards, show significant gaps between budgeted and actual staffing needs.
The anticipated outcome of the two programmes is highly likely to reduce or change what the triangulated approach of the establishment review suggested and therefore an interim position was recommended until the impact of the programmes are better understood as the work progresses. Flexibility of the use temporary staffing could still be applied should this be necessary.
Acute Inpatient Female Wards (Ward 1 & 5 Becklin Centre)
Ward 1 and 5 at the Becklin Centre are both twenty-two bedded female acute wards. The shift patterns include long days (12 hours) and a combination of early and late shifts (7.5 hours) with the majority of staff working long days.
The current staffing establishment is:
| Ward Type | Early/Late Shift | 9am – 5pm | Night Shift |
| Acute Inpatient Service | 3 x Registered Nurses
2 x HSW |
1 x Health Support Workers (Female Wards only) | 2 x Registered Nurses
2 x Health Support Workers |
In addition, each ward has the following
- Ward Manager x 1
- Ward Administrator x1
- Clinical Psychologist 0.5
- Psychology assistant 0.5
- OT Band 6 x 0.5
- OT band 5×1
- OTA x 1
- NA x 2
- Activity Coordinator x 1
- Peer worker x 1
- Practice Development 0.5 (3 WTW across the service)
The MHOST outcomes indicate that both ward budgets are not reflective of the recommended staffing WTE’s (whole time equivalents) excluding headroom. The total budget includes the additional roles such as AHP, Nursing Associates and Activity Coordinators.
| Ward | Total Budget WTE (excluding headroom 24%) | MHOST WTE Recommendation | Total worked included bank/agency Sept 23-Feb 24 |
| 1 | 26.2 | 33.6 | 36.62 |
| 5 | 26.4 | 41.3 | 43.24 |
The MHOST toolkit recommends an additional 7.4 WTE for Ward 1 above the existing budget and 14.9 WTE on Ward 5. The total worked has been slightly above the MHOST recommendation with both wards increasing the staffing numbers above the budgeted establishment through the use of bank/agency staffing.
Additional staffing above the planned establishment has been required within the female acute wards to meet perceived care needs. The female acute wards have used enhanced levels of observation and engagement daily and additional staff to facilitate escort status to support patient care. This has been predominantly in relation to service users who self-harm. This correlates with a higher number of incidents being reported in the female acute wards, with the highest proportion of these being self-harm, violence, and aggression incidents. The service is also experiencing an increase in complex physical health care needs and at times service users requiring periods of care at LTHT which has required additional staffing to support.
The below graphs detail the fill rate between March and August 2024 highlights that both wards are working over the budgeted establishment for Health Support Workers.
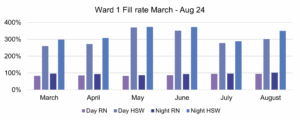

Acute Inpatient Male Wards (Ward 4 Newsam, Wards 3 and 4 Becklin Centre)
Ward 3 and 4 at the Becklin Centre are both twenty-two bedded male acute wards. Ward 4, Newsam Centre is a twenty-one bedded ward. The shift patterns include long days (12 hours) and a combination of early and late shifts (7.5 hours) with the majority of staff working long days. The MHOST outcomes indicate that the ward’s budget is not reflective of the current staffing WTE’s excluding headroom.
| Ward | Total Budget WTE (excluding headroom 24%) | MHOST WTE Recommendation | Total worked including bank/agency Sept 23-Feb 24 |
| 3 Becklin | 26.3 | 34.6 | 25.46 |
| 4 Becklin | 26.3 | 38.8 | 28.41 |
| 4 Newsam | 26.1 | 32.7 | 27.78 |
The total budget includes the additional roles such as AHP, Nursing Associates and Activity Coordinators. Both wards have the below roles which tend to work the core hours Monday to Friday 9am-5pm, this was reviewed as part of the establishment review. It was reported that the establishment numbers can struggle to meet clinical need either during core hours which is currently mitigated by the below roles or during the handover period from late to night shift.
This correlates with a higher number of incidents being reported in the afternoon (12:00 hrs to 17.59 hrs) followed by a combination of incidents on the late and night shift (18:00 hrs to 23.59 hrs). The requirement for additional staffing above the planned establishment has been required within the male acute wards. The male acute wards have experienced the need to use enhanced levels of observation and engagement and escort status to support patient care.
The MHOST toolkit recommends an additional 8.3 WTE on Ward 3, Becklin above the existing budget, 12.5 WTE on Ward 4, Becklin and 6.6 WTE on Ward 4, Newsam. The total worked has been slightly above the budgeted establishment.
The current staffing establishment is:
| Ward Type | Early/Late Shift | Night Shift |
| Acute Inpatient Male Wards | 3 x Registered Nurses/Nurse Associate
2 x Health Support Workers |
2 x Registered Nurses
2 x Health Support Workers |
In addition, each ward has the following
- Ward Manager x 1
- Ward Administrator x1
- Clinical Psychologist 0.5
- Psychology assistant 0.5
- OT Band 6 x 0.5
- OT band 5×1
- OTA x 1
- NA x 2
- Activity Co-Ordinator x 1
- Peer worker
- Practice Development 0.5 (3 WTE across the service)
The vacancy rate for Registered Nurses in Ward 4 Becklin was at 21.1% (3.3WTE) and 20% (3.2WTE) for Ward 4 Newsam in October 2024. This is predicted to reduce in the future with the recruitment of experienced Registered Nurses alongside preceptee recruitment. This will enhance the nursing leadership on both wards and reduce reliance on temporary staffing. The Registered Nurse vacancy rate for Ward 3 Becklin during this period was 17.9% with one of these vacancies due to be filled by a current Nursing Associate completing the Registered Nurse Training. Turnover was also low for this ward with the majority of Registered Nurses having 5-10 years’ experience working on this ward.
The below graphs detail the fill rate between March and August 2024 highlights that all wards are working over the budgeted establishment for Health Support Workers
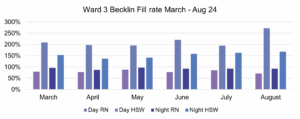

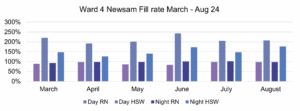
An increase to the establishment will reduce the reliance on temporary staff; substantive staff will provide both consistency and relational security which in turn will positively impact on the quality of care delivered. Research highlights that incidents such as aggression occurred more when there were fewer staff members in the milieu, there was an absence of regular staff, or when patients were unfamiliar with the staff. This will also reduce the workload of substantive staff who are required to provide high quality inductions to a large number of temporary staff.
Recommendations:
Acute Inpatient Service (Ward 1.3.4.5 Becklin and Ward 4 Newsam)
The interim recommendation is to increase the establishment by 1 x Band 3 Practitioners per shift (early, late and night). Band 3 roles are to be determined in a skill mix review and are likely to be a combination of roles such as Health Support Worker, Activity Coordinators and Peer Workers. Current Activity Coordinators and Nursing Associates will be integrated into the safer staffing numbers to support this increase of an additional practitioner per duty.
This will be reviewed at the next annual establishment review alongside evaluating the impact of the programme of works currently underway. The use of the temporary workforce will continue to provide flexibility should this be necessary as work progresses. However, it is essential that the use of bank staffing is monitored and the impact evaluated to inform any changes required should the impact not have the effect anticipated.
It is anticipated that the majority of Registered Nurse vacancies will be filled by Q3 2025/2026 as the cohort of Newly Qualified Nurses join the Trust in coming months alongside those in the current recruitment pipeline,
A focused piece of work will also take place as part of the programme of works to understand how other roles can more effectively contribute to the ward establishment to reduce the reliance on increased staffing using the temporary workforce.
| Ward Type | Early/Late Shift | 9am – 5pm | Night Shift |
| Acute Inpatient Female Service | 3 x Registered Nurses
3 x HSW |
1 x Health Support Workers (Female Wards only) | 2 x Registered Nurses
3 x Health Support Workers |
| Ward Type | Early/Late Shift | Night Shift |
| Acute Inpatient Male Wards | 3 x Registered Nurses/Nurse Associate
3 x Health Support Workers |
2 x Registered Nurses
3 x Health Support Workers |
Anticipated Outcomes:
- Embeds a foundation for higher quality care and sustainable workforce planning
- Improved clinical effectiveness
- Reduction in incidents through consistent care and relational security
- Builds resilience and responsiveness during transition including where engagement is required for the programme of works
- Reduces financial spend on temporary staffing
- Allows the programmes of work to progress and ability to understand the impact
Mount Ward 2
It was identified through the triangulated approach that there was a recommended need to increase the safer staffing numbers on this ward by x 1 Band 3. However, further discussions following the launch of the ETOC programme and other service initiatives have led to pausing the recommendation.
This will be reviewed at the next annual establishment review alongside evaluating the impact of the programme of works currently underway. The use of the temporary workforce will continue to provide flexibility should this be necessary as work progresses.
It is anticipated that the majority of Registered Nurse vacancies will be filled by Q3 2025/2026 as the cohort of Newly Qualified Nurses join the Trust in coming months alongside those in the current recruitment pipeline.
A focused piece of work will also take place as part of the programme of works to understand how other roles can more effectively contribute to the ward establishment to reduce the reliance on increased staffing using the temporary workforce.
Wards delivered by the Provider Collaborative
Business cases to the relevant Provider Collaborative have been developed reflecting the recommendations detailed in this report for clinical areas funded by the Provider Collaborative, this includes YCED, Clifton House and Red Kite View.
In response to this, an uplift in establishment at Clifton House, Riverfields was agreed as per recommendation to increase the staffing establishment by x 1 Band 3 on a night duty.
Further work to review the clinical models for YCED and RKV and Ward 5 Newsam were agreed before further decisions are made due to potential changes to the service specifications and the clinical model and pathway. The use of the temporary workforce will continue to provide flexibility should this be necessary as work progresses.
Summary
The importance of annual establishment reviews is to ensure the organisation is satisfied that the staffing establishment is set at an appropriate level. The reviews focused on identifying whether the current planned establishments across LYPFT inpatient wards remained appropriate to deliver safe and effective care through the application of the triangulated approach, including the use of MHOST data, quality indicators and professional judgement. These were conducted using a range of data, ensuring that MHOST, quality indicators and professional judgement were triangulated.
It was found that many wards were routinely utilising excess staffing above that of their agreed baseline establishments. It was acknowledged that this does not automatically lead to the need for an increase in establishment and in some clinical areas the review of clinical practice, skills and competencies were required before further consideration of any increase to staffing is recommended.
The staffing establishment review has enabled evidence-based recommendations to be made to increase the staffing establishment across the service is some clinical areas. However, the recommendations have been made at a time when significant workstreams which are linked to the Trust’s 14 priorities are commencing, which will in turn impact on staffing and workforce.
As a result, interim or alternate recommendations have been made acknowledging the possibility that the impact of these initiatives may result in a different outcome. A recommendation for the five wards across the Acute Inpatient Service has been made to increase the number of staff on each duty to enable the service to deliver safe and effective care. In additional, a recommendation was made to increase the establishment within Clifton House, Riverfields which was agreed with the Provide Collaborative and is now in situ.
The remainder of wards have been reviewed and the staffing establishment concluded as either appropriate, further work required or a pause on the recommendations until the significant programmes of work progress and the impact understood. Flexibility of the use temporary staffing could still be applied should this be necessary.
Sign off and Governance
The establishment review has been shared through the appropriate governance forums within LYPFT including the Executive Management Team forum. The paper was tabled at the Financial Performance Group and Finance and Performance Committee in September 2025 with approval to fund the posts and support the financial uplift required.
An assurance statement from the Director of Nursing is enclosed (Appendix 1)
The board are asked to:
- Note and be assured by the content of the paper
- Support the recommendations as outlined in the paper
Alison Quarry
Deputy Director of Nursing
16 September 2025
Appendix 1
Statement of assurance
I, Nichola Sanderson, as the Executive Director of Nursing and Professions can confirm that the nursing staffing establishment review for 2024/2025 has been completed in accordance with the National Quality Board (NQB) and the Developing Workforce Safeguards framework.
The review has incorporated
- Evidence based workforce planning tools
- Professional clinical judgement
- Analysis of patient acuity, dependency and outcomes
- Engagement with Finance, HR, and Clinical and Operational Leadership
- Consideration of current and projected service demands
Based on the findings and triangulated data, I am satisfied that the proposed staffing establishments are:
- Safe and appropriate to meet patient care needs
- Financially and regulatory sustainable
- Aligned with regulatory expectations and quality standards
I therefore formally sign off this review and recommend its submission to the Trust Board for assurance and approval.
Signed
Nichola Sanderson
Cover sheet for Guardian of Safe-working Hours Q1 Report
- Paper title: Guardian of Safe Working Quarterly Report Quarter 1: 1st April 2025 to 30th June 2025
- Date of meeting: 25 September 2025
- Presented by: Chris Hosker – Medical Director
- Prepared by: Rebecca Asquith – Guardian of Safe Working Hours
This paper supports the Trust’s strategic objective/s (SO):
- SO2 – We provide a rewarding and supportive place to work.
This paper relates to the Trust’s strategic risks (SR):
-
- SR1 – Quality including safety assurance processes
- SR3 – Culture and environment for the wellbeing of staff
- SR5 – Adequate working and care environments
Executive summary
The purpose of this report is to give assurance to the board that doctors in training are safely rostered and that their working hours are compliant with the terms and conditions of service (TCS) of the 2016 contract. Key points to note are:
- There have been 7 exception reports, with no breaches leading to a GOSW fine and 0 patient safety issues recorded in this period.
- Resident Doctors Forum met on 25th April 2025 with opportunity for feedback from Core and Higher Trainee representatives, as well as continued review of ERs and rota gaps.
Do the recommendations in this paper have any impact upon the requirements of the protected groups identified by the Equality Act? State below, ‘Yes’ or ‘No’. No.
If yes, please set out what action has been taken to address this in your paper.
Recommendation
The Board of Directors are asked:
- To agree that this report provides an assurance level for the systems in place to support the working arrangements of the 2016 Contract and TCS for the junior doctors working in the Trust and that they are meeting their objective of maintaining safe services
- To provide constructive challenge where improvement could be identified within this system.
Guardian of Safe Working Hours Report – Quarter 1: 1st April 2025 to 30th June 2025
1 Executive Summary
The purpose of this quarterly report is to give assurance to the board that doctors in training are safely rostered and that their working hours are compliant with the resident doctors contract 2016 and in accordance with resident doctors terms and conditions of service (TCS). The report includes the data from 01.04.2025 to 30.06.2025.
2 Quarter 1 Overview
| Vacancies | There are a total of 45 Core Training posts and 2 NIHR posts. There are a total of 34 Higher Training posts. All schemes are full. | ||||||
| Rota Gaps | April 2025 | May 2025 | June 2025 | ||||
| PRS | Middle Tier | PRS | Middle Tier | PRS | Middle Tier | ||
| Gaps
|
16 | 27 | 26 | 24 | 27 | 24 | |
| Internal Cover | 12 | 27 | 18 | 24 | 21 | 24 | |
| Agency cover | 0 | 0 | 0 | 0 | 0 | 0 | |
| Unfilled
|
4 | 0 | 8 | 0 | 6 | 0 | |
| Fill Rate
|
75% | 100% | 70% | 100% | 78% | 100% | |
| Reasons for Rota Gaps | Sickness (4) Vacant (5)
Off rota (3) Special absence (4) |
Sickness (4)
Vacant (9) Off rota (7) Left trust (4) Special leave (1) LTFT (2) |
Sickness (5)
Vacant (6) LTFT (5) Off rota (4) Left trust (6) |
Vacant (8)
Off rota (6) Left trust (5) LTFT (5) |
Sickness (9)
Vacant (14) LTFT (3) Left trust (1) |
Sickness (1)
Vacant (12) Off rota (6) Left trust (4) LTFT (1) |
|
| Comments
|
Rota gaps arise for various reasons including sickness, gaps arising from Less Than Full Time working patterns, rota gaps, and other leave including parental leave or special leave.
The Psychiatry Resident Rota (1st tier) is covered by FY2 and CT doctors. Of the shifts that were uncovered, 17 of these were night shifts and 1 was an evening shifts. The middle tier rota (2nd / middle tier) is covered by Higher Trainee doctors and continues to have a high fill rate. |
||||||
| Exception reports (ER)
|
There were 7 exception reports in total during the reporting period.
– One ER related to the delay in a (middle tier) resident doctor getting their rest due to completion of a MHA assessment, with delay contributed by lengthy wait for trust taxi. This has been fed back to the Medical Directorate and no further action required at this time. – Three ERs related to loss of educational opportunity through being unable to join ALPS due to acuity of work on the PRS rota. MEC continue to liaise with doctors when this occurs and whereby there have been 2+ missed opportunities, alternative arrangements to regain the learning experience where possible are made. – One ER related to loss of educational opportunity to attend psychotherapy supervision due to clinical commitments. This was escalated to the DME who has liaised with the Clinical Supervisor. – Two ERs related to claims for additional time worked at the end of a normal working day, due to the need to attend to an urgent physical health assessment. Both were settled with TOIL. |
||||||
| Fines | No fines were levied in this reporting period.
The total fine fund as of the end of the 2024-2025 year is £262.15 and sits within a GOSW cost centre. Spending from such funds will be agreed via the RDF. |
||||||
| Patient Safety Issues
|
None | ||||||
| Resident Doctor Forum (RDF) | The meeting held during the Q1 reporting period took place on 25th April 2025
– It was agreed to update the ‘Opt Out’ forms (forms completed by resident doctors to voluntarily opt out of European Working Time Directive) to explicitly state that locum work cannot be undertaken during contractually mandated rest periods. All updated forms were then recirculated for completion by resident doctors wishing to opt out. – It was noted that whereby a final ARCP takes place ‘out of sync’ for a resident doctor, the deanery have stated that they will remain in post as a trust doctor which has implications with regards their contract and Responsible Officer. Such ‘out of sync’ ARCPs may be more likely to occur when trainees work Less Than Full Time. The LTFT champion will highlight this to doctors to increase awareness. Any issues related to this should be raised with the Deanery and RO. – ERs were discussed (those occurring and detailed in Q4 report) – The RDF Terms of Reference were reviewed and agreed. – Proposed changes to Exception Reporting processes were discussed, but with limited information shared from the BMA and NHS Employers to further inform plans in this regard. It has been added as a standing agenda item. – The GOSW shared information about the role of the FTSUG and opportunities for them to present more about their role at the RDC and HTC. – The next RDF was scheduled for 18th July 2025. |
||||||
3 Conclusion
Exception Reporting has now been in place within the Trust since 2016 with the first ER being made in 2017. We continue to work with resident doctors and clinical supervisors to ensure that we are developing a culture where ERs are positively received and used as a mechanism to effect change. Examples of this includes the agreed process for MEC to oversee any missed educational opportunities related to ALPS and offer additional opportunities where required, and also more recent agreements via the RDF precipitated by ERs (in the last financial year) which were associated with breaches in the T+Cs and issuing of fines. Through MEC colleagues, the RDF, and GOSW attendance at induction for new starters, we continue to support the position that doctors are encouraged to work according to the T+Cs for their own safe practice and the safe care of patients. GOSW fines have been levied in the last financial year, but not in Q1 of this financial year. Spending of such fine monies will be agreed through the RDF. There are anticipated changes to the Exception Reporting processes in the near future as per the new ‘Framework Agreement’, however further guidance to support implementation of this is yet to be provided by the BMA and NHS Employers. Updated TCS are expected to be released in September 2025.
4 Recommendations
The Board of Directors are asked:
- To agree that this report provides an assurance level for the systems in place to support the working arrangements of the 2016 TCS for the resident doctors working in the Trust and that they are meeting their objective of maintaining safe services
- To provide constructive challenge where improvement could be identified within this system
Dr Rebecca Asquith
GMC 7151560
Guardian of Safe Working Hours
Chair’s Report from the Workforce Committee meeting on 7 August 2025
- Paper title: Chair’s Report from the Workforce Committee meeting on 7 August 2025
- Date of meeting: 7 August 2025
- Presented by: Zoe Burns-Shore, Non-executive Director and Chair of the Workforce Committee
- Prepared by: Rose Cooper, Deputy Head of Corporate Governance
This paper supports the Trust’s strategic objective/s (SO):
- SO2 – We provide a rewarding and supportive place to work.
This paper relates to the Trust’s strategic risk/s
- SR3 – Culture and environment for the wellbeing of staff
Committee details:
- Name of Committee: Workforce Committee
- Date of Committee: 7 August 2025
- Chaired by: Zoe Burns-Shore, Non-executive Director
Alert – items to alert the Board to:
- No items to alert the Board to.
Advise – items to advise the Board on
The Committee received an update on the Trust’s progress against the Workforce Race Equality Standard (WRES) and Workforce Disability Equality Standard (WDES) for the period 2024/25. The Committee discussed the reduced likelihood of ethnically diverse staff being appointed from shortlisting compared to white staff and heard what targeted work was planned to address this, supported by the new Head of Equality, Diversity and Inclusion. The Committee also discussed the increased likelihood of ethnically diverse staff entering the formal disciplinary process. The Committee noted that there had been only 10 formal disciplinary cases over 2024/25 which was a reduction compared to the previous year and acknowledged that this was a positive step forward. The Committee then noted that in 2024/25 four of the 10 individuals entering the formal disciplinary process were ethnically diverse staff. The Committee understood that due to the small number of cases overall in 2024/25, the dataset was not statistically significant and therefore it was difficult to draw conclusions from it; however, it was recognised that the issue of ethnically diverse staff being overrepresented in statistics around disciplinary cases was a historic one and therefore it was important to continue to give this issue focused attention. The Committee supported the WRES and WDES action plan provided in the report and agreed to review an update on progress at its December 2025 meeting.
The Committee approved the recommendations to support the implementation of Version 2 of the NHS Violence Prevention and Reduction Standard. The Committee noted that it had been difficult to translate the previous benchmarking and action plans onto the new Version 2 structure; however, the team were looking to complete the initial self-assessment against the new standards by the end of this year.
The Committee noted that, despite a significant amount of work in this area, sickness absence remained static at around 6%. The Committee highlighted that this was an ongoing challenge and noted that progress continued to be reported to the Board subcommittees via regular performance reports.
At the request of the Audit Committee, the Committee considered and agreed that the “Bullying and Harassment” audit should be undertaken separately from the “Retention and Wellbeing” audit and supported it being scheduled as part of the 2026/27 internal audit plan, or the 2025/26 plan if additional capacity became available.
Assure – items to provide assurance to the Board on
The Committee reviewed the Board Assurance Framework so that it could be mindful of its responsibility to assure that Strategic Risk (SR) 3 was being adequately controlled through the course of the meeting. The Committee was assured that SR3 was being adequately controlled; considered whether it was receiving assurance on any gaps through the reports it was already receiving; and agreed that it did not require any further assurance on the way in which SR3 was being managed.
The Committee received a high-level summary of the Staff Survey Intention Planning Campaign following the delivery of the 2024 Staff Survey and Bank Staff Survey results. The Committee noted that the highest number of Intention Plans had been completed to date and acknowledged the hard work of the People Engagement Team to support Intention Planning across the Trust.
The Committee received the Restrictive Interventions Annual Report 2024-25 as per the request from the Quality Committee and considered the workforce challenges referred to in the report. The Committee agreed that these issues were already being addressed through existing workstreams and therefore no further action was required by the Committee. The Committee also heard about what measures were in place to support staff who needed to carry out restrictive practice. The Committee highlighted the assurance received from the report and noted that this reflected an improving culture around restrictive practice that was becoming embedded at the Trust.
The Committee received the Time and Attendance Management Internal Audit Report at the request of the Audit Committee and noted the outcome of significant assurance.
The Committee received the summary of the Gender Pay Gap report for 2024/25 and was pleased to note the positive year-on-year reduction in the median gender pay gap figure.
Refer – Items to be referred to other Committees:
- No items to refer to other committees.
Recommendation
The Board of Directors is asked to note the update provided.
Cover sheet for Equality Annual Report (including WRES and WDES and Gender Pay Gap)
- Paper title: Equality Annual Report (including WRES and WDES and Gender Pay Gap)
- Date of meeting: 25 September 2025
- Presented by: Fiona Sherburn, Associate Director HR/OD
- Prepared by: Fiona Sherburn, Associate Director HR/OD
This paper supports the Trust’s strategic objective/s (SO):
- SO3 – We use our resources to deliver effective and sustainable services.
This paper relates to the Trust’s strategic risks (SR):
- SR3 – Culture and environment for the wellbeing of staff
Executive summary
This paper provides a summary update on the Trust’s progress against the Workforce Race Equality Standard (WRES) and Workforce Disability Equality Standard (WDES) for the period 2024/25. The paper includes details of progress against current priority areas and actions. It also summarises the gender pay gap report 2024/25, which as required has been reported on the Trust’s website.
Although there is no legal obligation to report on the comparable staff survey data for LGBTQ+ this is included in this report for completion along with proposed actions to address the issues raised by LGBTQ+ staff.
The data shows that there is still significant work to be done to improve the experiences at work by staff with protected characteristics
The WRES comprises nine metric areas with only four showing a favourable change. This is a deterioration from last year when six of the metrics showed a favourable change.
The WDES is comprised of 10 metrics, with three of these have shown a favourable change. This is a decline in performance from last year when nine of the metrics showed a favourable change.
The Trust’s GPG reporting data shows a positive year on year reduction in the median gender pay gap figure. On average women within the Trust now earn 99p for every £1 that men earn when comparing median hourly pay (0.7%). In 2021/2022 women earned 95p for every £1 that men earned when comparing median hourly pay (5.3%). This shows a 4.6% reduction in the median GPG.
Although there is currently no national benchmark available for sexual orientation or gender identity – an analysis of the relevant staff survey questions highlights that there are two areas where the results are unfavourable for LGBTQ+ when compared with the previous year.
For transgender staff one indicator indicates a significantly poorer experience when compared to cisgender staff, which is for the experiences of harassment, bullying or abuse from service users, their relatives or members of the public, which is +15.2% for cisgender.
A comprehensive action plan is proposed to address the issues identified in this paper. The actions align with the Trust’s People Plan, the Messenger Report and the NHS Ten Year Plan.
Do the recommendations in this paper have any impact upon the requirements of the protected groups identified by the Equality Act?
Yes – the proposed action plan set out in the paper should have a positive impact on staff with protected characteristics.
Recommendation
The Board is asked to:
- Note the 2025 WRES and WDES results.
- Receive assurance that the WRES and WDES data was submitted in May 2025 in line with submission requirements and that actions published on the Trust website in September 2025 to meet statutory reporting requirements.
- Note the Gender Pay Gap (GPG) figures for 2024-25 and to receive assurance that the GPG data was submitted in line with reporting requirements.
- Support the inclusion of GPG data by pay band for the first time and the inclusion of LGBTQ+ data which provides a more comprehensive overview of the experiences of staff with protected characteristics
- Support the proposed actions to address the issues raised in the data.
Equality, Diversity and Inclusion Report
September 2025
- Executive Summary
This paper provides a summary update on the Trust’s progress against the Workforce Race Equality Standard (WRES) and Workforce Disability Equality Standard (WDES) for the period 2024/25. The paper includes details of progress against current priority areas and actions. It also summarises the gender pay gap report 2024/25, which as required has been reported on the Trust’s website.
Although there is no legal obligation to report on the comparable staff survey data for LGBTQ+ this is included in this report for completion along with proposed actions to address the issues raised by LGBTQ+ staff.
The WRES and WDES are national standards that aim to respond to lack of progress in race and disability equality in the NHS. The data identifies areas that aim to address equality gaps and improve the workplace experience for our substantive ethnically diverse and disabilities/LTHCs (long term health conditions) colleagues.
The WRES comprises nine metric areas with only four showing a favourable change. This is a deterioration from last year when six of the metrics showed a favourable change.
The areas showing an unfavourable change are as follows: –
- The likelihood of white staff being appointed following shortlisting has increased from 2.00 to 2.90. This is disappointing as it represents a further increase from 2023/24. Contributing factors are detailed within the paper, including a large increase in the number of ethnically diverse candidates who were shortlisted in 2024/25 which can be viewed as positive and a potential result of proactive recruitment within local communities.
- The likelihood of ethnically diverse staff entering the formal disciplinary process has increased from a likelihood of 1.93 to 2.37. Again, contributing factors are detailed, including the overall reduction in the number of formal disciplinary cases, attributable to the new Disciplinary processes, which is positive.
- The percentage difference between the organisation’s Board voting membership and its overall workforce (BME representation) shows an under-representation. Although the number of BME staff on the board remains the same there has been a year-on-year increase in workforce ethnicity representation, which in itself is positive.
- Percentage of staff experiencing harassment, bullying or abuse from staff in last 12 months has increased. For ethnically diverse staff it has increased slightly from 17.1% to 17.8%.
- Percentage of staff who in the last 12 months personally experienced discrimination from their manager/team leader or colleagues has increased from 10.2% to 13.25%.
The WDES is comprised of 10 metrics, with three of these have shown a favourable change. This is a decline in performance from last year when nine of the metrics showed a favourable change.
The areas where there has been unfavourable change is as follows:
- There has been a slight increase in the number of staff with disabilities/LTHCs experiencing harassment, bullying or abuse from patients, service users and the public. This has increased from 25.74% to 26.73%.
- The percentage of staff with disabilities/LTHCs staff experiencing harassment, bullying or abuse from colleagues has seen a small increase from 17.16% to 17.64%
- The percentage of staff who believe that the Trust provides equal opportunities for career progression or promotion has decreased from 59.3 % to 53.2%.
- The percentage of staff who say they have felt pressure from their manager to come to work, despite not feeling well enough to perform their duties has increased from 14.85% to 15.9 %.
- The percentage of staff satisfied with the extent to which the organisation values their work, has reduced further from 47.4% to 45.65%
- The percentage of staff saying their employer has made reasonable adjustments to enable them to carry out their work has decreased from 86.54% to 80.9%.
- The staff engagement score has decreased from 6.90% to 6.69%.
The Trust’s GPG reporting data shows a positive year on year reduction in the median gender pay gap figure. On average women within the Trust now earn 99p for every £1 that men earn when comparing median hourly pay (0.7%). In 2021/2022 women earned 95p for every £1 that men earned when comparing median hourly pay (5.3%). This shows a 4.6% reduction in the median GPG.
The GPG incudes a bonus pay calculation which is based on the NHS Clinical Excellence Awards (CEA) payments awarded to medical consultants within the Trust. Although it is positive to note that for a second year, the median bonus gender pay gap is zero, indicating parity in terms of the award distribution to both women and men it should be noted that for this reporting period an equal distribution award round was in operation which has influenced the median GPG figure.
The mean bonus data identifies that women’s average bonus pay was 18.36% higher than men’s. Across our workforce a total of 0.6% of women and 1.8% of men received bonus pay. As noted in last year’s paper, there continue to be several historic CEA awards which are recurrently paid each year. The gender distribution of bonus pay and the historic CEA awards has influenced this increase due to a small number of female medical consultants who have been in receipt of an award over a long period of time compared with a larger number of male medical consultants whose length of service is much shorter and therefore they have only been in receipt of an award for the past couple of years.
Although there is currently no national benchmark available for sexual orientation or gender identity – an analysis of the relevant staff survey questions highlights that there are two areas where the results are unfavourable for LGBTQ+ when compared with the previous year i.e.
- There has been an 8.5% decline in LGBTQ+ staff believing that LYPFT provides equal opportunities for career progression/promotion.
- There has been 9.1% decline in LGBTQ+ staff feeling satisfied with the extent to which LYPFT values their work.
- Five of the seven metrics indicate significantly poorer experiences compared to heterosexual staff.
For transgender staff one indicator indicates a significantly poorer experience when compared to cisgender staff, which is for the experiences of harassment, bullying or abuse from service users, their relatives or members of the public, which is +15.2% for cisgender.
- WRES and WDES Performance Overview
2.1 WRES
The WRES is comprised of nine metric areas and a summary overview is provided below along with the Trust’s Workforce Race Equality Data.
Table 1 Trust’s Workforce Race Equality Data
A total of four out of the nine WRES standard metrics have shown favourable change from last year and full details are set out below.
Metric 1
Percentage of staff in Agenda for Change pay-bands or medical and dental subgroups and very senior managers (including Executive Board members) compared with the percentage of staff in the overall workforce.
The 2025 data shows that 25% of our workforce (excluding bank) are from an ethnically diverse background. This is an increase of 2.0% when compared to 2024 and is above the current 2021 Census figures for Leeds which identifies that 21% of the population are from an ethnically diverse background.
Whilst it is positive that there has been an increase in the percentage of ethnically diverse staff working for the Trust when compared to the census figure for Leeds, there is clearly further work to do to ensure that the Board properly reflects the workforce and this will need to be addressed through the recruitment process as and when board appointments arise.
“Relative Likelihood” WRES Metrics Two, Three and Four
The following three metrics indicate the likelihood of ethnically diverse (BME) candidates being appointed from shortlisting, staff entering a formal disciplinary process and staff accessing non mandatory training.
A figure of 1.0 suggests an equal position, however it is worth noting that the calculation of this data can be affected by small numbers.
Table 2
| WRES Metric | Metric Description | 2024 Score | 2025 score |
| 2 | Relative likelihood of white staff being appointed from shortlisting compared to that of BME staff being appointed from shortlisting across all posts. | 2.00 | 2.90 |
Table 2 identifies an unfavourable change in the likelihood of white staff being appointed from shortlisting compared to ethnically diverse staff. The ratio figure for 2025 indicates white staff being almost three times as likely to be appointed from shortlisting. This is an increase from 2024 which is very disappointing.
Table 2 identifies an unfavourable change in the likelihood of white staff being appointed from shortlisting compared to ethnically diverse staff. The ratio figure for 2025 indicates white staff being almost three times as likely to be appointed from shortlisting. This is an increase from 2024 which is very disappointing.
There has been a large increase in the number of ethnically diverse applicants (1164) who were shortlisted and therefore invited to interview when compared to data from 2024 (731), which in itself is positive. Potential reasons for this increase include focused recruitment activity such as, values-based recruitment, job fairs targeting areas with diverse populations and other activity as part of our widening participation work.
It is also worth noting that the Trust commenced a pilot of flipped recruitment for early career roles in April 2024. Fourteen roles have been appointed to using this method; 50% of applicants and 47% of successful candidates were ethnically diverse. This method of recruitment pre-screens applicants, removing the need for shortlisting from a Trac application form and, ensures that those individuals invited to interview are high quality candidates.
Work is underway to pilot this approach for experienced and qualified healthcare support workers in older people’s services. If this approach is successful in attracting and appointing more ethnically diverse staff, then the recruitment team will work with services to embed this approach into business-as-usual recruitment processes.
Running alongside this work further analysis will be undertaken to understand why this increase in short-listing of ethnically diverse applicants is not leading to more ethnically diverse applicants being appointed.
In 2024/25 there was a total of 377 appointments (excluding bank), where ethnicity was known. Of this total 28% of staff appointed were ethnically diverse and 72% were white. This is above the ethnicity representation of our overall workforce at 25%.
Table 3
| WRES Metric | Metric Description | 2023 Score | 2024 score |
| 3 | Relative likelihood of BME staff entering the formal disciplinary process compared to White staff. | 1.93 | 2.37 |
There has again been an unfavourable change in the likelihood of ethnically diverse staff entering the formal disciplinary process. During 2024/25 there were a total of 10 individuals who entered the formal disciplinary process, with four of these being ethnically diverse colleagues.
It is important to acknowledge that the total number of formal disciplinary cases has decreased significantly, from 25 in 2023/24 to 10 in 2024/25. This reduction reflects a positive cultural shift towards a restorative and reflective approach to managing conduct, rather than a punitive one. However, the over representation of ethnically diverse staff in formal processes remains a concern.
The introduction and embedding of the revised Disciplinary Policy in 2022, including the early-stage Decision-Making Group (DMG) process, has been a key driver in this reduction. The DMG enables early, balanced consideration of cases and has helped to de-escalate issues before they reach formal stages. To strengthen safeguards against bias, Cultural Inclusion Ambassadors are now included in all DMG discussions regardless of the nature of the allegation or the ethnicity of the individual involved. This is a deliberate step to ensure that unconscious bias does not influence early decision-making.
The data suggests that while the overall number of cases has declined, the equity of outcomes has not improved at the same pace. Further analysis is needed to understand whether the DMG process is effectively mitigating bias and supporting fair decision-making across all staff groups.
Table 4
| WRES Metric | Metric Description | 2023 Score | 2024 score |
| 4 | Relative likelihood of white staff accessing non-mandatory training or CPD | 1.00 | 0.75 |
The likelihood figure continues to show that ethnically diverse staff are more likely to access non-mandatory training or CPD. This is postive and reflects the continued focus across the Trust to develop and deliver relevant training and CPD to support our diverse workforce. Career development sessions are an example of this, which have been developed through discussion with the Equality and Diversity team and our staff networks to inform the focus and content.
Metrics 5 to 8 Staff Survey Responses
All two of the four of the national staff survey WRES metric areas show an unfavourable change, as detailed in Table 5 below.
Table 5
| WRES Staff Survey Metrics | 2021 | 2022 | 2023 | 2024 | Year on Year Change | Against Sector Average | ||
| % Staff- All Ethnic Groups | ||||||||
| % experiencing harassment, bullying or abuse from patients, relatives or the public in the last 12 months | 37.9% | 35.8% | 33.7% | 30.7% | -3.0% | Favourable | 31.6% | Better |
| % experiencing harassment, bullying or abuse from staff in the last 12 months | 22.8% | 22.5% | 17.1% | 17.8% | +0.7% | Unfavourable | 21.2% | Better |
| % believing that the organisation provides equal opportunities for career progression or promotion | 42.7% | 42.0% | 51.9% | 52.8% | +0.9% | Favourable | 51.0% | Better |
| % experiencing discrimination at work from manager/team leader or other colleagues in the last 12 months | 13.3% | 11.8% | 10.2% | 13.2% | +3.0% | Unfavourable | 13.2% | Same |
There has been an increase in the number of staff experiencing harassment, bullying or abuse from staff in the last 12 months as well as the number of staff experiencing discrimination at work from a manager or team leader or other colleagues in the last 12 months.
More positively there has been a decrease in the percentage of staff experiencing harassment, bullying or abuse from patients, relatives or the public in the last 12 months and an increase in the percentage of staff believing that the organisation provides equal opportunities for career progression or promotion.
All measures are the same or above our sector average.
Table 6
| WRES Metric | Metric Description | 2024 Score | 2025 score |
| 9 | Percentage difference between the organisation’s Board voting membership and its overall workforce (BME representation). | -%7.7 | -9.2% |
Table 6 compares the difference between the Board voting membership and our overall ethnically diverse workforce. The ethnicity representation in our workforce has increased year on year. If this trend continues and the the number of ethnically diverse voting members of the Board remains the same, the disparity will show a year on year increase. The recruitment of a more diverse board is something that will need to be considered as Board members step down.
2.2 WDES
The WDES is comprised of ten metric areas.
Metric 1
This metric looks at the percentage of staff in Agenda for Change pay-bands or medical and dental subgroups and very senior managers (including Executive Board members) compared with the percentage of staff in the overall workforce.
The 2025 data shows that 12.0 % of our workforce (excluding bank) have a disability or long-term health condition. This is an increase of 2.5% when compared to 2024.
“Relative Likelihood” WDES Metrics Two and Three
Table 7
| WDES Metric | Metric Description | 2024 Score | 2025 score |
| 2 | Relative likelihood of non-Disabled staff being appointed from shortlisting compared to that of Disabled staff being appointed from shortlisting across all posts. | 0.9.2 | 1.1 |
The probability figure illustrates that non-disabled staff are more likely to be appointed from shortlisting compared to disabled staff.
In 2024/25 there were a total of 375 appointments where Disability status was known. Of this total 12% were Disabled, this is above the disability representation of our overall workforce at 10.7%
Table 8
| WDES Metric | Metric Description | 2023 Score | 2024 score |
| 3 | Relative likelihood of Disabled staff entering the formal capability process compared to non-Disabled staff. | 0 | 0 |
This metric is based on data from a two-year rolling average (2022/23 and 2023/24). During this period there were no disabled and two non-disabled staff entering the formal capability process on the grounds of performance.
Metrics 4 to 8 Staff Survey Responses
Seven out of the nine staff survey WDES metric areas show an unfavourable change, as detailed in Table 9 below.
There has been a significant decrease in the following two areas:-
The percentage of staff saying that their employer has made reasonable adjustments to enable them to carry out their work from 86.5% to 80.9%.
The percentage of staff believing that the organisation provides equal opportunities for career progression or promotion has decreased from 59.3 % to 53.2 %.
The two areas of improvement are as follows:
The percent of staff experiencing harassment, bullying or abuse from managers in the last 12 months has decreased from 8.7% to 8.0.% and the percentage saying the last time that they experienced harassment bullying or abuse at work, they or a colleague reported it increased from 59.2% to 66.6%.
Data will be shared with teams and services to inform their staff and to gather member views in relation to potential improvement actions and areas of planning at team level to inform staff survey intention plans and discussions have commenced with the DaWN staff network to share the findings with them and identify improvement actions.
Overall three of the metrics are worse than the sector average and six better than the sector average.
Table 9
| WDES Staff Survey Metrics | 2021 | 2022 | 2023 | 2024 | Year on Year Change | Against Sector Average | ||||
| % Staff with a Long-Term Condition (LTC) or illness | ||||||||||
| % experiencing harassment, bullying or abuse from patients, relatives or the public in the last 12 months |
31.2% |
30.9% |
25.7% |
26.7% |
1.0% |
Unfavourable |
26.6% |
Worse |
||
| % experiencing harassment, bullying or abuse from managers in the last 12 months | 12.2% | 9.6% | 8.7% | 7.9% | -0.8% | Favourable | 11.4% | Better | ||
| % experiencing harassment, bullying or abuse from colleagues in the last 12 months |
22.3% |
19.7% |
17.2% |
17.6% |
0.4% |
Unfavourable |
17.9% |
Better |
||
| % saying the last time that they experienced harassment bullying or abuse at work, they or a colleague reported it | 66.9% | 59.4% | 59.2% | 66.6% | 6.9% | Favourable | 62.9% | Better | ||
| % believing that the organisation provides equal opportunities for career progression or promotion |
50.0% |
57.4% |
59.% |
53.2% |
-6.1% |
Significantly Unfavourable |
55.13% |
Worse |
||
| % who felt pressure from their manager to come to work when not feeling well enough to work | 17.0% | 16.2% | 14.9% | 15.9% | 1.0% | Unfavourable | 17.9% | Better | ||
| % satisfied with the extent to which their organisation values their work | 41.5% | 49.9% | 47.4% | 45.7% | -1.7% | Unfavourable | 44.3% | Better | ||
| % saying their employer has made reasonable adjustments to enable them to carry out their work | N/A | 83.5% | 86.5% | 80.9% | -5.6% | Significantly Unfavourable |
79.6% | Better | ||
| WDES 9a – Staff Engagement score (0-10). | 6.76 | 6.81 | 6.90 | 6.69 | 0.20 | Unfavourable | 6.74 | Worse | ||
Table 10
| WRES Metric | Metric Description | 2024
Score |
2025
Score |
| 10 | Percentage difference between the organisation’s Board voting membership and its overall workforce (Disabled representation). | 6.6 % |
This metric compares the difference between the Board voting membership and our overall Disabled workforce. The data positively identifies that our voting Board membership is over representative of our Disabled workforce by 12.9%.
- Gender Pay Gap
The Equality Act 2017 Regulations require all organisations that employ more than 250 staff to publish their gender pay gap (GPG) information annually.
Data for 2024/2025 GPG reporting period has been submitted in line with reporting requirements. A summary of the results for Leeds and York Partnership Foundation Trust can be found on the Government’s gender pay gap web pages.
The GPG differs from equal pay in the following way. Equal pay deals with pay differences between men and women who carry out the same jobs, similar jobs or work of equal value. It is unlawful to pay people unequally because they are a man or a woman. The gender pay gap shows the differences in the average pay gap between men and women.
Table 11
| GPG Reporting Period | 2020/2021 | 2021/2022 | 2022/2023 | 2023/24 |
| Average Gender Pay Gap- MEAN | 11.4% | 10.9% | 10.3% | 10.5% |
| Average Gender Pay Gap- MEDIAN | 5.9% | 5.3% | 3.1% | 2.3% |
Median Gender Pay
Our latest data indicates a substantial positive year on year reduction in the median gender pay gap figure as detailed in Table 11 above. On average women within our Trust now earn 98p for every £1 that men earn when comparing median hourly pay (2.3%).
In 2020/2021 women earned 94p for every £1 that men earned when comparing median hourly pay (5.9%). This identifies a 3.6% reduction in the median GPG.
Mean Gender Pay
Our latest mean (average) gender pay figure indicates a slight negative increase of 0.2% when compared to 2022/2023 data. When comparing the data detailed in Table 11, it shows less than a 1% reduction in the mean GPG over the four-year data period.
It should be noted that although utilising mean averages are useful, that very high or low hourly pay figures can substantially influence and distort the overall figure as detailed in the section below.
Gender Pay Quartile Profile
Table 12 below shows the percentage of females in each pay quartile. The lower quartile represents the lowest salaries in the Trust and the upper quartile represents the highest salaries. The Trust employs more women than men in every quartile. 77.5% of females are employed in the lower quartile, compared to 67.1% in the upper quartile, a 10.4% difference which research has identified can have a negative effect particularly on the mean gender pay gap figure.
Table 12
| Quartile | 2020/2021 | 2021/2022 | 2022/2023 | 2023/24 |
| 1 Lower Quartile | 74.3% | 65.5% | 74.4 | 77.5% |
| 2. Lower middle quartile | 72.4% | 74.2% | 72.5% | 69.1% |
| 3. Upper middle quartile | 73.9% | 73.4% | 73% | 72.9% |
| 4. Upper quartile | 66% | 74.2% | 66.2% | 67.1% |
Bonus Gender Pay Gap
Table 13
| Bonus GPG Reporting Period | 2020/2021 | 2021/2022 | 2022/2023 | 2023/2024 |
| Average Bonus Gender Pay Gap- MEAN | 33% | 20.3% | 15.7% | 16.8% |
| Average Bonus Gender Pay Gap- MEDIAN | 66% | 37.5% | 36.8% | 0% |
The bonus pay calculation is based on the NHS Clinical Excellence Awards (CEA) payments and processes awarded to medical consultants within the Trust. Table 13 above highlights the mean and median bonus pay linked to clinical excellence awards.
Median Bonus Gender Pay Gap
It is positive to note that the median bonus gender pay gap has reduced to 0% indicating increased parity in terms of the distribution to both females and males. It should be noted that for this reporting period an equal distribution award round was in operation which has influenced the median GPG figure.
Mean Bonus Gender Pay Gap
The latest mean bonus data identifies a small increase of 1.1% in the bonus gender pay gap. There continue to be several historic CEA awards which are recurrently paid each year. These will influence and account for this identified increase.
Gender Pay Gap by pay band
Table 14
| AfC Pay Grade | Female | Male | Difference | Pay Gap % |
| Band 1 | 20.77 | -20.77 | ||
| Band 2 | 12.72 | 12.82 | 0.10 | 0.76 |
| Band 3 | 14.34 | 15.03 | 0.69 | 4.61 |
| Band 4 | 14.56 | 14.45 | -0.11 | -0.79 |
| Band 5 | 17.32 | 17.61 | 0.29 | 1.64 |
| Band 6 | 21.63 | 22.17 | 0.53 | 2.41 |
| Band 7 | 24.77 | 25.09 | 0.32 | 1.28 |
| Band 8 – Range A | 28.67 | 29.08 | 0.41 | 1.42 |
| Band 8 – Range B | 33.13 | 33.51 | 0.37 | 1.11 |
| Band 8 – Range C | 40.10 | 41.72 | 1.62 | 3.87 |
| Band 8 – Range D | 48.99 | 46.05 | -2.94 | -6.39 |
| Band 9 | 57.14 | 53.00 | -4.14 | -7.81 |
| Other | 43.82 | 46.57 | 2.75 | 5.90 |
| Total | 29.08 | 29.76 | -1.61 | 0.67 |
The above table shows that there is a gender pay gap in favour of men in every Agenda for Change pay band except 8D, 9 and medical staffing (other).
Further analysis will be undertaken to better understand what the underlying cause of the pay gap is so that appropriate and more targeted interventions can be put in place.
- LGBTQ+
Although there is currently no national benchmark available for sexual orientation or gender identity the data from the relevant staff survey are included for completeness in terms of this EDI update.
Table 15 – Staff Survey Question
| LGBO | 2023 | 2023 | 2024 | 2024 | YoY 23/24 |
Comp 2024 |
| Question | LGBO | Straight | LGBO | Straight | LGBO+ vs SRT | |
| – % of staff who experienced at least one incident of harassment, bullying or abuse from: Patients / service users, their relatives or other members of the public. | 26.9% | 21.7% | 25.8% | 20.3% | -1.2% | 5.4% |
| % of staff who experienced at least one incident of harassment, bullying or abuse from: Managers. | 6.4% | 6.0% | 4.9% | 5.4% | -1.4% | -0.5% |
| – % of staff who experienced at least one incident of harassment, bullying or abuse from: Other colleagues. | 16.0% | 11.0% | 18.8% | 13.1% | 2.7% | 5.7% |
| – % of staff saying they, or a colleague, reported harassment, bullying or abuse. | 58.0% | 60.3% | 59.7% | 68.8% | 1.7% | -9.1% |
| % of staff who believe that their organisation provides equal opportunities for career progression / promotion. | 62.9% | 60.3% | 54.4% | 62.4% | -8.5% | -8.0% |
| – % of staff who have felt pressure from their manager to come to work despite not feeling well enough to perform duties. | 61.6% | 49.5% | 61.7% | 50.6% | 0.1% | 11.2% |
| – % of staff satisfied with the extent to which their organisation values their work. | 56.6% | 55.0% | 47.5% | 53.6% | -9.1% | -6.1% |
The data highlights that there are two areas where the results are unfavourable for LGBO when compared with the previous year i.e.
- There has been an 8.5% decline in LGBO staff believing that the organisation provides equal opportunities for career progression/promotion.
- There has been 9.1% decline in LGBO staff feeling satisfied with the extent to which the organisation values their work.
- Five of the seven metrics indicate significantly poorer experiences compared to heterosexual staff.
Table 16 – Gender Identity
This is the first year the report has included comparable data for transgender staff.
Overall, five of the areas show significant favourable results for transgender staff and one area i.e. experiences of harassment, bullying or abuse from service users, their relatives or members of the public, which is +15.2% for cisgender is significantly poorer for transgender staff.
| Gender Identity Same as Birth – Yes/No | 2023 | 2023 | 2024 | 2024 | YoY 23/24 |
Comp 2024 |
| Question | No – T | Yes – C | No – T | Yes – C | Cis vs Trans | |
| – % of staff who experienced at least one incident of harassment, bullying or abuse from: Patients / service users, their relatives or other members of the public. | 33.3% | 22.4% | 35.7% | 20.5% | 2.4% | +15.2% |
| – % of staff who experienced at least one incident of harassment, bullying or abuse from: Managers. | 6.7% | 5.9% | 0.0% | 5.3% | -6.7% | -5.3% |
| – % of staff who experienced at least one incident of harassment, bullying or abuse from: Other colleagues. | 20.0% | 11.0% | 14.3% | 13.6% | -5.7% | 0.7% |
| – % of staff saying they, or a colleague, reported harassment, bullying or abuse. | N/A | 59.2% | N/A | 66.6% | N/A | |
| – % of staff who believe that their organisation provides equal opportunities for career progression / promotion. | 37.5% | 60.9% | 57.1% | 61.4% | +19.6% | -4.3% |
| – % of staff who have felt pressure from their manager to come to work despite not feeling well enough to perform duties. | 68.8% | 50.3% | 50.0% | 52.3% | -18.8% | -2.3% |
| – % of staff satisfied with the extent to which their organisation values their work. | 25.0% | 55.3% | 57.1% | 52.2% | 32.1% | 4.9% |
- Next Steps and Proposed Actions
5.1 WRES, WDES and LGBTQ+ Actions
Overall the data from the WRES, WDES as well as the data for LGBTQ+ staff highlights significant areas for improvement if the Trust is to improve the experience of our ethnically diverse workforce and staff with disabilities/long term health conditions.
During 2024/25, work was undertaken to address issues raised in last year’s WRES/WDES, including the following: –
- Appointment of a new substantive head of EDI who will start in September 2025
- Recruitment of ten new cultural inclusion ambassadors
- Roll-out of Values Based Recruitment across key services
- Piloted a cultural competence training programme
- Piloted flipped recruitment for apprentices in a number of services including estates and finance
- From July 2025 it is mandatory for recruiting managers to undertake the Trust’s recruitment and selection training and renew it every three years. Failure to do so will prohibit them from recruiting staff for their service or team.
Despite this work the Trust’s performance has deteriorated in a number of areas over the last 12 months which means that there needs to be a real focus given to this area of work going forward to improve things for staff. Including data from LGBTQ+ staff further highlights the need for action to improve the experience of staff with protected characteristics at work.
Reflecting on the data and feedback from staff it is proposed to focus on the following actions for the next 12 months: –
- Establish a Strategic EDI group that will provide clear leadership to the EDI agenda, set the strategic direction and ensure actions are being delivered upon. This group will be chaired by the Chief People Officer and the first meeting will take place in September 2025.
- Develop a Resolving Concerns policy and procedure to replace the current approach to grievance and bullying and harassment complaints. This will be a further step to prevent unnecessary escalation of issues into formal process to improve the experience of our colleagues. The new approach will also ensure a timely response to complaints of bullying and harassment within the Trust. The review will take place during 2025 with a planned launch by the end of March 2026.
- Communicate and publicise the range of support (which is significant) that is in place to support staff with disabilities/long term health conditions through a comprehensive communication plan which will be delivered by October 2025 and also integrated into the new starter process and wellbeing conversations.
- Develop a new workplace adjustment process, including guidance for managers put in place by the end of December 2025 with a focus on ensuring staff receive any workplace adjustments in a timely manner.
- Undertake a listening exercise with the staff networks to understand how the Trust can better support staff with disabilities/LTHCs, ethnically diverse staff and LGBTQ+ staff with their career development. From October 2025
- Review the Disability Confident Assessment and develop an appropriate action plan by the end of December 2025 to ensure that the Trust fully meets the standard.
- Provide some dedicated support to the Trust’s Staff networks to support their development and growth which is an essential component on helping staff feel valued and supported. The networks also provide a valuable source of knowledge and peer support. From October 2025
- Review the recruitment and selection training to ensure that the existing unconscious bias training is as robust as possible, ensuring recruitment panels are reflective. By March 2026
- Reflect on the review of the Cultural Competence Training pilot develop a plan to deliver this training to staff across the Trust – with a focus on hotspot areas. By March 2026
5.2 Gender Pay Gap Actions
Across the NHS we know that structural aspects of the workforce are contributing to the overall the gender pay gap with many move women working at lower pay bands than men.
As highlighted above there is further work to do analyse the data further – by gender and pay band to get a better understanding of the gender pay gap issues within the Trust and how we can address them.
In addition to this data analysis, we will undertake the following actions to address our Gender Pay Gap:
· Develop our talent management strategies to support the development of women into more senior roles. By April 2026
· Raise the profile of the benefits of Flexible Working across the Trust through a range of methods, including communication briefings, promoting the flexible working toolkit. On-going 2025/26
· Promote the career development workshops to encourage all staff to reach their full potential. On-going 2025/26
· Promote the bite sized and online training to ensure development can be easily accessed by those working part time and flexible work patterns. On-going 205/26
- Governance and Assurance
The Trust’s WRES and WDES data was submitted in line with reporting requirements i.e. by 31 May 2025 and the data and revised action plan published in September 2025 on the Trust’s website as per national reporting requirements.
The data will be shared with the staff networks, who have played a key role in contributing to our improvement actions, as well as the Equality, Diversity and Inclusion, Civility and Respect and Strategic Resourcing groups, to ensure that this data feeds into their planning process for improvements.
Work is now underway to develop a reporting framework on the ethnicity pay gap in line with national requirements and further information about this will be provided to the Board when we are clear about the expectations and reporting requirements.
In addition, further work will be done to improve data analysis of the staff survey data so that we can drill down further and explore issues around intersectionality so that we can better understand where the hotspot areas to provide targeted support and appropriate interventions.
- Recommendations
The Board is asked to:
- Note the 2025 WRES and WDES results.
- Receive assurance that the WRES and WDES data was submitted in May 2025 in line with submission requirements and that actions published on the Trust website in September 2025 to meet statutory reporting requirements.
- Note the Gender Pay Gap (GPG) figures for 2024-25 and to receive assurance that the GPG data was submitted in line with reporting requirements.
- Support the inclusion of GPG data by pay band for the first time and the inclusion of LGBTQ+ data which provides a more comprehensive overview of the experiences of staff with protected characteristics
- Support the proposed actions to address the issues raised in the data.
Chair’s Report from the Mental Health Legislation Committee meeting on 5 September 2025
- Paper title: Chair’s Report from the Mental Health Legislation Committee meeting on 5 September 2025
- Date of meeting: 25 September 2025
- Presented by: Kaneez Khan, Non-executive Director and Chair of the Mental Health Legislation Committee
- Prepared by: Kieran Betts, Corporate Governance Officer
This paper supports the Trust’s strategic objective/s (SO):
- SO1 – We deliver great care that is high quality and improves lives.
- SO2 – We provide a rewarding and supportive place to work
- SO3 – We use our resources to deliver effective and sustainable services.
This paper relates to the Trust’s strategic risk/s
- SR1 – Quality including safety assurance processes
- SR3 – Culture and environment for the wellbeing of staff
- SR5 – Adequate working and care environments
- SR7 – Plan and deliver services that meet the health needs of the population we serve
Committee details:
- Name of Committee: Mental Health Legislation Committee
- Date of Committee: 5 September 2025
- Chaired by: Kaneez Khan, Non-executive Director
Alert – items to alert the Board to:
- No items to alert the Board to.
Advise – items to advise the Board on
- The Committee discussed the Trust’s target for a Mental Health Act Assessment to be started within three-hours of a Service User’s admission. It agreed that feedback would be given to the Section 136 and Crisis Teams from the Committee to improve record-keeping in this area, with the hope that this would demonstrate the Trust was compliant with this target in many cases. It was also agreed that data regarding compliance with this target would also be included in future quarterly Mental Health Legislation Activity Reports received by the Committee so this area could be monitored.
- The Committee noted that the Trust was missing the ethnicity data of approximately 6% of its service users as reported in the Q1 2025-26 Mental Health Legislation Activity Report and discussed why this was the case. It noted that having a full picture of all service users ethnic background would be important to deliver the Trust’s Health Equity Strategy. It agreed that it would question at the September 2025 Board of Director’s Meeting which Board Committee would be responsible for monitoring and driving improvement in this area, as this issue fell within the remit of multiple Board Committees.
- The Committee noted the results of the follow-up audit on the Mental Capacity Act (MCA) Assessments and Best Interest Decision documentation conducted by the Mental Health Legislation Team. It was reported that there were still significant issues to address in this area as some of the documentation sampled lacked the detail required to meet the legal standards specified by the MCA. The Committee was reassured that there were some improvements demonstrated in this area in more recent document samples and actions being taken by the Mental Health Legislation Team to improve training and conduct more targeted audits in the future but noted that there was still significant room for improvement. It agreed that it would continue to monitor developments in this area and noted the request made by the Mental Health Legislation Team for this area to be reaudited by internal audit as part of the 2027-28 internal audit plan.
Assure – items to provide assurance to the Board on
- The Committee received feedback from the MHLOSG. It discussed the following issues in detail:
- Delays in referrals to AMHPs which was causing the Emergency Duty Team to become involved in routine cases. The Committee was assured that the Mental Health Legislation Team had written to all consultants in the Trust as well as attending the Clinical Improvement Forum to help address this issue.
- The reduced capacity of the Section 136 Suite as a result of incidents of violence and aggression. The Committee noted that the Nursing Directorate had plans to redesign the Suite to address this issue.
- The Committee received feedback from the Mental Health Act Managers (MHAMs) Forum. It noted that the MHAMs had not raised any concerns regarding the “Paper Hearing” pilot which the Trust had implemented on 1 September 2025 for a period of six-months, which allowed the need for a formal MHAMs Hearing to be circumvented when the decision to extend a service users detention or Community Treatment Order (CTO) was not being contested. The Committee agreed to monitor the rollout and feedback from this pilot.
- The Committee received the Mental Health Legislation Activity Report for Q1 2025-26 and was assured that the plans in place were sufficient to ensure ongoing compliance with all Mental Health Legislation. It noted the following:
- That the use of CTOs had increased in the quarter.
- The Trust’s ethnically black inpatient population had decreased in the period so that the Trust’s inpatient population and the general population of Leeds was near parity. Conversely, the ethnically Asian inpatient population had increased so that individuals from this background were overrepresented compared to the general population of Leeds.
- There were some delays in MHAMs Hearings caused by the unavailability of responsible clinicians or legal representatives. The Committee noted that the Mental Health Legislation Team was working to address these issues. It also noted that the Trust was increasing its number of responsible clinicians which was also hoped to help address this issue
- The Committee completed its Committee Effectiveness review and was assured that no changes were required to be made to its Terms of Reference or practices as a result of this review.
Refer – Items to be referred to other Committees:
- No items to refer to other committees.
Recommendation
The Board of Directors is asked to note the update provided.
Cover sheet for Board of Directors Terms of Reference
- Paper title: Board of Directors Terms of Reference
- Date of meeting: 25 September 2025
- Presented by: Merran McRae, Chair
- Prepared by: Clare Edwards, Associate Director of Corporate Governance
This paper supports the Trust’s strategic objective/s (SO):
- SO3 – We use our resources to deliver effective and sustainable services.
This paper relates to the Trust’s strategic risks (SR):
- SR1 – Quality including safety assurance processes
- SR2 – Delivery of the Quality Strategic Plan
- SR3 – Culture and environment for the wellbeing of staff
- SR4 – Financial sustainability
- SR5 – Adequate working and care environments
- SR6 – Digital technologies
- SR7 – Plan and deliver services that meet the health needs of the population we serve.
Executive summary
As part of governance processes, there is a requirement for the Board to review its Terms of Reference on an annual basis. Given the function and role of the Board has not materially changed, the content remains the same with no amendments made.
The template has been updated to ensure it is in line with the current administrative templates in place.
Do the recommendations in this paper have any impact upon the requirements of the protected groups identified by the Equality Act? No
Recommendation
The Board of Directors is asked to approve the Terms of Reference.
Leeds and York Partnership NHS Foundation Trust
Board of Directors
Terms of Reference
(Approved by the Board of Directors on 26 September 2024)
The Trust has Standing Orders for the practice and procedures of the Board of
Directors (Annex 8 of the Constitution). For the avoidance of doubt, those Standing
Orders take precedence over these Terms of Reference, which do not form part of
the Trust’s Constitution.
1. Name
Board of Directors
2. Composition of the Board
The membership of the Board of Directors is determined in accordance with Section
19 of the Trust’s Constitution and shall comprise both executive and non-executive
directors acting as a unitary Board.
Members:
- A non-executive chair
- A minimum of 4 and a maximum of 6 other non-executive directors
- A minimum of 4 and a maximum of 6 executive directors
The above shall be considered as the composition of the Board, provided at least
half the Board excluding the Chair of the Trust comprises non-executive directors
who have been determined by the Board to be independent.
For clarity the executive directors who are members of the Board of Directors are:
- Chief Executive
- Chief Financial Officer
- Medical Director
- Director of Nursing and Professions
- Chief Operating Officer
- Director of People and Organisational Development
All members of the Board of Directors shall have one full vote each, with the chair
having a second or casting vote should the need arise.
The Board of Directors will appoint one of the independent non-executive directors to
be the Senior Independent Director. In consultation with the Chair of the Trust, the
Council of Governors will also appoint one of the non-executive directors to be the
Deputy Chair of the Trust.
Members of the Board of Directors must ensure that wherever possible they attend
every Board meeting (including extraordinary Board meetings when convened). An
explanation of non-attendance should be made to the Chair of the Trust. Attendance
at meetings will be monitored by the Associate Director for Corporate Governance
and shall be reported to the Chair of the Trust and the Council of Governors on a
regular basis. Attendance will also be reported annually in the Annual Report.
The Board may invite non-members to attend its meetings on an ad-hoc basis,
where it considers this to be necessary and appropriate, and this will be at the
discretion of the Chair.
| Title | Role in the meeting | Attendance guide |
| Associate Director for Corporate Governance | Shall be the Board Secretary, attending all meetings of the Board of Directors and providing appropriate advice and support to the Chair and Board members. This will include ensuring agreement of the agenda with the Chair, collation of papers, taking minutes and keeping proper records of the meeting including any actions to be carried forward. It shall also include the preparation of those corporate governance papers pertaining to the Board of Directors. | Every meeting
|
In the absence of the Associate Director for Corporate Governance the Deputy Trust
Board Secretary will deputise.
2.1 Governor Observers
The role of the governor at public Board of Directors’ meetings is to observe, rather
than to be part of its work. They are not part of the formal membership of the Board,
nor are they classed as in attendance. Governors are invited to observe the Board
meetings to get a better understanding of the work of the Trust and to observe nonexecutive directors appropriately challenging the executive directors for the
operational performance of the Trust.
At the meeting the governor observer will be required to declare any interest they
may have in respect of any of the items to be discussed (even-though they are not formally part of the discussion). Governors will receive an electronic copy of the
public Board papers prior to the meeting. Governor observers will be invited to the
public meetings only, by the Corporate Governance Team.
2.2 Associate Non-executive Directors
Associate Non-executive Directors will be invited to attend Board of Directors’
meetings (both public and private meetings) as part of their induction. They will be in
attendance at the meeting, in the capacity of observer only, unless invited to
contribute (in exceptional circumstances) by the Chair. This is so the integrity of the
unitary Board and the accountability of the substantive members of the Board is
maintained.
Associate NEDs will be invited to the public and private meetings by the Corporate
Governance Team and will be sent copies of all Board papers.
3. Quoracy
Number: No business shall be transacted at a meeting of the Board of Directors
unless at least one third of the whole number of the members of the Board is
present, including at least one executive director and one non-executive director.
Deputies: Where, exceptionally, an executive director is absent from a meeting they
may not normally send a deputy in their place. However, attendance to cover
absences will be at the discretion of the chair and will be agreed in order to ensure
the Board has access to appropriate advice and information. In these circumstances
the deputy attending will not have any voting rights and will be recorded as in
attendance. Where there are formal acting up arrangements in place the person
acting-up into an executive director role may attend and will assume the voting rights
of the director they are acting up for. In such circumstances they will be recorded as
a member of the Board.
Non-quorate meetings: Non-quorate meetings may go forward unless the chair
decides otherwise. Any decisions made by the non-quorate meeting must be
reviewed at the next quorate meeting.
4. Meetings of the Board
All meetings shall be held in public except where matters are deemed confidential on
the grounds of commercial sensitivity, personal issues or matters that could cause
harm to individuals by the nature of their content. Such matters will be discussed in
a separate closed session which will not be attended by members of the public. Any
person attending the private Board meeting will be at the discretion of the Chair.
Meetings may be held face-to-face or remotely as is considered appropriate.
Remote meetings may involve the use of the telephone and / or electronic
conference facilities.
A full set of papers comprising the agenda, minutes and associated reports and
papers will be sent to all directors within the timescale set out in Standing Order
3.3.1 in Annex 8 of the Constitution (or as agreed by the Chair).
Copies of the public and private agendas will be sent to members of the Council of
Governors prior to any meeting.
The public agenda papers and minutes of each public meeting shall be displayed on
the Trust’s website
Frequency: Meetings of the Board of Directors shall be held at such times as the
Board may determine. The frequency of meetings shall be agreed by the Board of
Directors and will normally be bi-monthly (excluding August and December). The
Board may agree to vary that frequency. This shall not preclude urgent meetings
being convened at any time in accordance with Standing Order 3.2 in Annex 8 of the
Constitution.
The Board has also agreed to hold Strategic Discussion meetings which will normally
be scheduled in the months between the formal Board meetings (excluding August).
These meetings will be used as protected time to discuss in greater detail matters
that may emerge from the formal meetings as well as those which will further inform
the work of the Board. Holding a strategic discussion session does not preclude any
part of this meeting being constituted as an urgent meeting should the need arise.
Urgent meetings: Urgent meetings shall be convened in accordance with Standing
Order 3.2 in Annex 8 of the Constitution.
Minutes: The Associate Director for Corporate Governance, acting in the capacity as
Trust Board Secretary shall take the minutes. They will ensure these are presented
to the next full business meeting of the Board of Directors for agreement. Minutes
may be held either electronically or in paper format but always in a way that is
accessible and preserves the continuous record of the meeting.
5. Authority
The Trust is required to establish a Board of Directors in accordance with the NHS Act
2006 (as may be amended by the H&SC Act 2012), and paragraph 21 of the Trust’s
Constitution. All members of the Board shall act collectively as a unitary Board with each
member having equal liability.
6. Role of the Board of Directors
6.1 Purpose of the Board of Directors
The principle purpose of the Trust is the provision of goods and services for the purposes
of the health service in England. The purpose of the Board is to ensure the provision of
those health services it is commissioned to provide; that these are delivered in line with its
strategy; that services are safe and effective and are provided to a high quality; to provide
leadership and direction to the organisation; and to ensure it is governed effectively with
appropriate systems processes and procedures in place.
The Board will achieve this by:
- Setting and overseeing the strategic direction of the organisation within the overall
policies and priorities of the Government, the Trust’s regulators, and its
commissioners, having taken account of the views of the Trust’s members (through
the Council of Governors), and the wider community - Ensuring accountability by holding the organisation to account for the delivery of
the strategy; and through seeking assurance that systems of control are robust and
reliable - Shaping a positive culture for the organisation
- Being assured on the work of the executive directors
- Taking those decisions that it has reserved to itself.
The Trust has a Board, made up of executive and non-executive directors, which
exercises all the powers of the Trust (as the entity) on its behalf, but the Board may
delegate any of those powers to a sub-committee of the Board (made up of
directors) or to an executive director. (Arrangements for the reservation and
delegation of powers are set out in the Reservation of Powers to the Board of
Directors and Council of Governors and Schedule of Decisions/Duties Delegated by
the Board of Directors (known as the Scheme of Delegation) and the Terms of
Reference of its sub-committees.
6.2 Guiding principles for members (and attendees) when carrying out the duties of
the Board
In carrying out their duties, members of the Board and any attendees at the meeting
must ensure they act in accordance with the values of the Trust, which are:
- We have integrity
- We are caring
- We keep it simple.
6.3 Duties of the Board of Directors
The duties set out below shall not preclude the Board of Directors from reserving powers
and duties to itself. These powers and duties shall be set out in the Scheme of
Delegation, and, for the avoidance of doubt, where there is a conflict the Scheme of
Delegation will take precedence over these Terms of Reference.
The duties of the Board of Directors are to:
- Set the values and strategic direction of the Trust; and ensure the Trust’s Strategy
and any supporting strategic plans are reviewed as necessary - Provide leadership to the Trust to promote the achievement of the Trust’s ‘Principal
Purpose’ as set out in the Constitution (i.e. the provision of goods and services for
the purposes of health services in England), ensuring at all times that it operates in
accordance with the Constitution and the conditions of the license as issued by
NHS England - Engage as appropriate with the Trust’s membership through the Council of
Governors - Promote and develop appropriate partnerships with other organisations in
accordance with the Trust’s values and strategic direction - Oversee the implementation and achievement of the Trust’s strategic objectives
- Agree the Trust’s Operational Plan
- Ensure the Trust has adequate and effective governance and risk management
systems in place, including responsibility and oversight of the Board Assurance
Framework - Monitor the performance of the Trust and ensure the executive directors manage
the Trust within the resources available in such a way as to: ensure the safety of service users and the delivery of high-quality care; ensure the continuous improvement of services; protect the health and safety of service users, employees, visitors and all others to whom the Trust owes a duty of care; make effective and efficient use of the Trust’s resources; comply with all relevant regulatory and legal requirements; maintain high standards of ethical behaviour, corporate governance and personal conduct in the business of the Trust; maintain the high reputation of the Trust both with reference to local system and place stakeholders, and the wider community. - Receive and consider high-level reports on matters material to the Trust detailing
in particular, information and action with respect to: service user and carer experience; clinical quality including safety; performance, including performance against targets and contracts; human resource matters; the identification and management of risk; financial performance; matters pertaining to the reputation of the Trust. - Promote teaching, training, research and innovation in healthcare to a degree
commensurate with the Trust’s teaching status - Review and approve any declarations/compliance statements to regulatory bodies
prior to their submission - Review and adopt the Trust’s Annual Report and Accounts
- Act as corporate trustee for the Leeds and York Partnership NHS Foundation Trust
Charitable Trust Funds.
7. Relationships with other groups and committees
The Board of Directors may delegate powers to formally constituted sub-committees
(whose membership is made up of directors). Without prejudicing the formation of any
other sub-committee the Board has formally constituted the following:
- Audit Committee
- Quality Committee
- Mental Health Legislation Committee
- Workforce Committee
- Finance and Performance Committee
- Remuneration Committee
- Nominations Committee
The Executive Team will support the Chief Executive in the implementation of the Board’s
decisions and will facilitate the efficient and effective working of the Board of Directors by
considering and responding to those matters referred to it. The Board of Directors’ reporting structure is detailed below.
8. Duties of the Chair
The Chair of the Board of Directors shall be the Chair of the Trust. In the
absence of the Chair of the Trust, (or in the event of them declaring a conflict
of interest in an agenda item) the Deputy Chair shall chair the meeting.
Should the Deputy Chair not be available (or where they too have also
declared a conflict of interest in an agenda item), the meeting shall be chaired
by one of the other independent non-executive directors.
The chair of the Board shall be responsible for:
- Providing leadership to the Board of Directors
- Enabling directors to make a full contribution to the affairs of the Board
of Directors ensuring that the Board acts as a cohesive team - Ensuring the key appropriate issues are discussed by the Board of
Directors in a timely manner - Ensuring the Board of Directors has adequate support and necessary
data on which to base informed decisions and monitor that such
decisions are implemented - Providing a conduit between the Council of Governors and the Board of
Directors - Agreeing the agenda with the Associate Director for Corporate
Governance - Directing the conduct of the meeting ensuring it operates in accordance
with the Trust’s values - Giving direction to the minute taker
- Ensuring all attendees have an opportunity to contribute to the
discussion - Ensuring the agenda is balanced and discussions are productive, and
when they are not productive they are efficiently brought to a
conclusion - Checking the minutes.
In the event of there being a dispute between any ‘groups’ in the hierarchy (in
the case of the Board, this would be between the Board and it’s committee) it
will be for the chairs of those ‘groups’ to ensure there is an agreed process for
resolution; that the dispute is reported back to the ‘groups’ concerned; and that
when a resolution is proposed the outcome this is also reported back to the
‘groups’ concerned for agreement.
In the event of their being a dispute between the Board of Directors and the
Council of Governors, a dispute resolution process is set out in the Trust’s
Constitution.
9. Review of the Terms of Reference and Effectiveness
The Terms of Reference shall be reviewed and ratified at least annually by the
Board of Directors.
In addition to this the Board of Directors must also carry out an assessment at
least annually of how effectively it is carrying out its duties and act on any
improvements agreed.